6. Self-harm and suicidal behaviour of young people aged 14-15 years old
6. Self-harm and suicidal behaviour of young people aged 14-15 years old
Galina Daraganova


- In an emergency, call 000
- Lifeline www.lifeline.org.au ph. 13 11 14
- Kids Help Line (5-25 years) kidshelpline.com.au ph. 1800 55 1800
6.1 Background
Introduction
Self-harm and suicidal behaviour is an important public health concern attracting attention from policymakers and mental health practitioners all around the world (Hawton, Saunders, & O'Connor, 2012). Among young people who engage in this behaviour, the age of onset of self-harm is usually between 11 and 15 years, while for suicidal behaviour it is between 15 and 17 years (Evans, Hawton, & Rodham, 2004; Hawton, et al., 2012; Lawrence et al., 2015; Jacobson & Gould, 2007; Klonsky & Muehlenkamp, 2007; Kumar, Pepe, & Steer, 2004; Muehlenkamp & Gutierrez, 2004; Nixon, Cloutier, & Aggarwal, 2002; Nock & Prinstein, 2004; Muehlenkamp, Claes, Havertape, & Plener, 2012).
Taken together, self-harm and suicidal behaviour account for a considerable portion of the disability burden and mortality among adolescents (Gore et al., 2011). According to worldwide statistics, self-harm has been reported as one of the top five reasons for acute medical admissions (Haq, Subramanyam, & Agius, 2010) and suicide is the second leading cause of death among 15-20 year olds (World Health Organization [WHO], 2014). In Australia, similar trends have been observed, with around one in ten (11%) 12-15 year olds reporting ever been involved in self-harming behaviour (Lawrence et al., 2015), and suicide being the leading cause of death among 15-24 year olds in 2012 (Australian Bureau of Statistics [ABS], 2016). Therefore, understanding the epidemiology and risk factors of self-harm and suicide-related behaviour is crucial for developing effective prevention programs.
Self-harm: epidemiology and correlates
Self-harm (self-injury) is commonly defined as a deliberate act of hurting yourself physically as a way of releasing painful emotions or communicating personal distress to others (Royal Australian and New Zealand College of Psychiatrists [RANZCP], 2009; Klonsky, 2007). While the act of self-harm might not have a fatal intent, severe cases of physical injury can result in death (Conner, Langley, Tomaszewski, & Conwell, 2003).
The majority of young people who engage in self-harming behaviours hide their injuries and may never seek help from medical or other services as a result of their self-harming acts (Moran et al., 2012; Muehlenkamp et al., 2012). Therefore, population estimates of the prevalence of self-harm vary considerably depending on the source of information (i.e., hospital admissions records or general population surveys). Statistics on "hospitalised self-harm" are mainly available for severe cases of self-harm and do not include cases when adolescents are admitted to emergency departments, treated by paramedics attending a call-out or a general practitioner, or die prior to hospitalisation (Martin et al., 2009). According to different international studies, only 6-12.6% of those who had harmed themselves had presented to hospital, whereas the vast majority of self-harm acts remain invisible to professionals (McMahon et al., 2014).
General population surveys report more accurate lifetime prevalence rates of self-harm. The majority of prevalence studies report the lifetime rates of self-harm among adolescents to be between 15% and 30% (Baetens, Claes, Onghena, Muehlenkamp, & Grietens, 2011; Ross, Heath, & Toste, 2009; Whitlock et al., 2013; You, Leung, Fu, & Lai, 2011). Prevalence estimates for adolescents in the United States, for example, varied from 20% to 37% among young people aged 14-16 years old and was 7-8% among children aged 11-13 years old (Plener, Schumacher, Munz, Groschwitz, 2015). An epidemiological study of adolescents (age 14-17 years) in seven European countries and Australia found an average lifetime prevalence estimate of 17.8% and a 12-month prevalence of 11.5% for self-harm behaviour, with some variation across countries (Madge et al., 2008). According to the most recent Australian survey on the mental health of children and adolescents (Lawrence et al., 2015), 6.2% of 12-15 year olds have engaged in self-harming behaviour in the previous 12 months.
The prevalence rates of self-harm are the highest among adolescents and greater among girls than boys. As young people get older, the prevalence rates decrease and the gap between boys and girls reporting acts of self-harm narrows (Whitlock & Rodham, 2013). A study of individuals aged 12-15 years in Australian and US schools (Patton et al., 2007) found that the greater prevalence of self-harm among girls has been largely attributed to issues related to pubertal development, especially late or completed puberty, rather than chronological age (Hawton et al., 2012).1 Other factors associated with the increased risk of self-harm have been poor mental health or an underlying psychological or emotional problem (Haw, Hawton, Houston, & Townsend, 2001; Zubrick et al., 2016a); experience of bullying, domestic violence or abuse in childhood (Fisher et al., 2012; Lang & Sharma-Patel, 2011; Maniglio, 2011); poor peer and family relationships (Prinstein et al., 2010; Jarvi, Jackson, Swenson, & Crawford, 2013); stressful life events (Meltzer et. al, 2002); and engagement in risk-taking behaviours (Madge et al., 2011). Growing evidence reports also on a strong association between sexual orientation and non-suicidal self-harm, with non-heterosexual people being at higher risk of self-harm compared to heterosexual people (King et al., 2008). Interestingly, studies of self-harm predictors also find some notable variations by gender. For example, friends' engagement in self-harm and the parent-child relationship were risk factors of self-harm for girls but not for boys (Prinstein et al., 2010; Bureau et al., 2010).
The decrease in the prevalence rate of self-harm behaviour as young children grow older (around 20 years old and above) suggests that this behaviour ceases in most cases. However, recurrent self-harm increases the risk of accidental suicide and the likelihood of suicide-related behaviours, including attempted and completed suicide (Bergen et al., 2012).
Suicide-related behaviours: epidemiology and correlates
Suicide-related behaviour, including suicidal thoughts (also known as suicidal ideation), plans and attempts, is defined as self-destructive behaviour with the primary intent to end life (Hawton et al., 2012). Prevalence estimates of suicide-related behaviour among adolescents also vary depending on the source. The official statistics substantially under-report suicide rates due to misclassification of suicide in young people as undetermined or accidental cause of death (Gosney & Hawton, 2007). In 2011, the reported age-specific suicide rate for Australians aged 15-19 was 10 deaths per 100,000 (ABS, 2014). The prevalence estimates of suicide-related behaviours are mainly available via population-based studies. According to the second Australian Child and Adolescent Survey of Mental Health and Wellbeing in the previous 12 months, 8% of 12-15 year olds reported having suicidal ideation, 5% reported having a suicidal plan, and 3% reported attempting suicide (Lawrence et al., 2015). As suicide is uncommon before 15 years of age, statistics for children younger than 15 years are usually not reported.
Gender differences are also observed in the prevalence of suicide-related behaviours, with boys reporting higher rates of completed suicide, while girls report higher rates of other suicide-related behaviours (thoughts, plans and attempts). In the second national Australian sample of adolescents 12-15 years of age (Lawrence et al., 2015), 8% of girls and 3% of boys reported having suicidal ideations, 6% of girls and 2% of boys made suicidal plans, and 3% of girls and 1% of boys ever attempted suicide.
Different risk factors of suicide-related behaviours have been identified. Poor mental health (Houston, Hawton, & Shepperd, 2001; Fortune, Stewart, Yadav, & Hawton, 2007; Reinherz et al., 1995), risk-taking behaviour (Houston et al., 2001; Aseltine, Schilling, James, Glanovsky, & Jacobs, 2009), non-heterosexual orientation (Ryan, Huebner, Diaz, & Sanchez, 2009), childhood trauma or abuse (Fergusson, Boden, & Horwood, 2008), dysfunctional family dynamics and changes (Fergusson, Boden, & Horwood, 2007; Brent & Mann, 2005), poor peer dynamics (Klomek et al., 2009), poor emotion regulation capacity (Nock et al., 2013) and negative cognition (negative thoughts or beliefs that limit current functioning) (Muehlenkamp & Gutierrez, 2007) are the most common factors identified as likely candidates for explaining suicide-related behaviours (for review see Cash & Bridge, 2009).
The risk factors associated with suicide-related behaviours are similar to the risk factors associated with self-harm (Prinstein et al., 2008). While it has been well-established that engagement in self-harm is related to an increased likelihood of suicide, and this is particularly the case for those who get admitted to the emergency department or report recurrent self-harm (Bergen et al., 2012; RANZCP, 2009), not every person who self-harms goes on to attempt suicide. Moreover, a large proportion of young people engaged in self-harm are not intentionally suicidal and, in fact, describe self-harm as a way to avoid suicide (Hawton & James, 2005).
To develop effective prevention and early intervention strategies it is of crucial importance to obtain accurate prevalence data, understand distal and concurrent risk factors associated with acts of self-harm and attempted suicide, and identify any gender differences.2 Although a lot of research has been conducted in this area, there are still gaps that require further research. Firstly, population-based studies on prevalence rates of self-harm and suicide-related behaviour aggregated for 14-15 year olds are scant. The second national Child and Adolescent Survey of Mental Health and Wellbeing reports prevalence rates for 12-15 year olds (Lawrence et al., 2015). Given that self-harm and suicidal behaviour is less prevalent among 12-13 years olds, these aggregated estimates might underrepresent the prevalence rates for adolescents aged 14-15 years. Secondly, limited and inconsistent findings are available on key risk factors in the presence of various confounders. Finally, only a small number of studies have examined the distal predictors of self-harm and suicide-related behaviours.
Research questions
This chapter uses LSAC K-cohort data to address these gaps and, in particular, to examine risk factors associated with the onset of self-harm and suicidal behaviour. The key research questions explored in this chapter are:
1. What are the prevalence rates of self-harm and suicidal behaviour among 14-15 year olds and do the prevalence rates vary by gender?
2. What are the risk factors associated with self-harm?
3. What are the risk factors associated with suicide attempts after controlling for self-harm?
4. To what extent is poor socio-emotional health earlier in life associated with self-harm and suicide attempts at age 14-15 years?
After a description of the LSAC data and methods used, the results are organised as follows. First, the overview of prevalence rates of self-harm and suicide-related behaviours and relationships between these behaviours are presented. The overview is followed by a description of the analytical approach and the analysis of main risk and protective factors associated with self-harm and suicide attempts. The analytical section examines the association between earlier indicators of mental health measured at 10-11 and 12-13 years of age and engagement in self-harm and attempting suicide at 14-15 years. Gender-specific differences are discussed throughout the chapter. The chapter concludes with a discussion around key findings, limitations and future research.
6.2 Sample and measures
This section provides a brief description of the sample and key measures used. Other variables, and the methods used to analyse the data, are described in later sections of the chapter.
Sample
The focus of this chapter is the K cohort, Wave 6 data, when the LSAC study children were aged 14-15 years (n = 3,318). Given that this chapter examines self-harm and suicide-related behaviours, only adolescents who answered the relevant questions were included in the sample.3 There were 1,694 boys and 1,624 girls aged 14-15 years. In some analyses, both Wave 4 and 5 data were used. In that analysis, the sample was reduced to 1,591 boys and 1,548 girls.
Measures of self-harm and suicide-related behaviours
Self-harm
In LSAC, measures of self-harm were derived from the AVON Longitudinal Study of Parents and Children (ALSPAC): Life of a 16+ Teenager questionnaire (ALSPAC, 2007). Table 6.1 describes the questions and corresponding measures used in the analysis. It is worth noting that intent of self-harm was not specified. Also, no information was collected on methods of self-harm.
Suicide-related behaviour
Measures of suicide-related behaviours were derived from the National Survey of Mental Health & Wellbeing (ABS, 2007). Questions regarding suicide-related behaviour and corresponding measures used in this chapter are described in Table 6.2. No information was collected on methods of suicidal behaviour.
6.3 Prevalence rates of self-harm and suicidal behaviours
This section reports the prevalence rates of self-harm and suicide-related behaviours of 14-15 year olds.4 The prevalence rates are presented separately for boys and girls and overall. The significant differences in the prevalence estimates among boys and girls were tested using chi-square tests and reported if the corresponding confidence intervals did not overlap. All the analyses were performed using weighted data, adjusting for sample design and non-response.
Self-harm
The prevalence rates of thoughts of self-harm and acts of self-harm were 16% and 10%, respectively (Table 6.3). Half of the young people who thought about self-harm also reported engaging in self-harm (56%). The prevalence rates of thoughts and acts of self-harm among girls were 25% and 15%, respectively. More than half of the girls (60%) who reported thinking about self-harm also reported engaging in self-harm. A similar pattern was observed for boys, but their prevalence rates were significantly lower than the girls' rates (see Table 6.3). The prevalence rates of thoughts and acts of self-harm among boys were 9% and 4%, respectively. Notably, out of those boys who thought about self-harm, less than half reported engaging in self-harm (42%). This proportion was significantly lower in boys than it was in girls.
Notes: Statistical significance is reported if the 95% confidence intervals do not overlap [95CI].
Source: LSAC, K cohort, Wave 6
Suicidal behaviours
Table 6.4 reports the prevalence rates of suicidal behaviours for all 14-15 year olds and by gender. The 12-month prevalence rates of suicide ideation, plans and attempts were 9%, 7% and 5%, respectively. Two thirds (66%) of adolescents who attempted suicide did so once, one in five (22%) attempted two or three times, one in ten (9%) attempted four or five times, and six children attempted six or more times. Out of those who reported a suicide attempt, 16% reported that at least one of those attempts had resulted in them receiving treatment from a nurse or doctor.
Girls were also more likely to be involved in suicidal behaviour than boys. More than one in ten girls (12%) reported suicidal ideation, 9% reported developing suicidal plans, and 6% of girls reported at least one suicide attempt. Out of the girls who did attempt suicide, 59% tried once, 22% attempted two or three times, 15% tried four or five times, and four girls attempted six or more times. Around one in five girls who made a suicide attempt were treated by a nurse or doctor as a result of that attempt (18%).
Among boys, 6% reported suicidal ideation, 5% reported suicidal plans, and 4% reported at least one suicide attempt. Among those who had attempted suicide, a majority of boys had attempted only once (75%), and 14% were medically treated.
Notes: Statistical significance is reported if the 95% confidence intervals do not overlap [95CI].
Source: LSAC, K cohort, Wave 6
Among those who reported having thoughts about suicide in the previous 12 months, a majority also reported developing a suicide plan (56%) and 37% reported a suicide attempt (Table 6.5). Only one third of those who reported suicidal ideation did not report any other suicidal behaviours. Only four in ten with a plan also reported a suicide attempt, with 60% not going ahead with their plan.
Among those who reported a suicide attempt, almost 60% also reported planning suicide. That is, 40% of suicide attempts were unplanned. One in five adolescents who reported attempting suicide did not report having any suicidal ideation or plans. While there is not always "causal" order in suicidal ideation, plans and attempts, the findings provide an important insight into possible pathways of suicidal behaviour.
Notes: Statistical significance is reported if the 95% confidence intervals do not overlap [95CI].
Source: LSAC, K cohort, Wave 6
The rates reported in Table 6.5 were similar among boys and girls who reported suicidal ideation, but varied among those who reported a suicide attempt. Girls who reported a suicide attempt were more likely to also report developing a suicide plan than boys (69% vs 42%, respectively), resulting in 30% of unplanned attempts among girls versus 60% of unplanned attempts among boys. In contrast, boys who reported a suicide attempt were more likely than girls to also report no suicidal ideation and no suicide plans (36% vs 12%, respectively).
Pathways between self-harm and suicidal behaviour
The relationships between self-harm and suicide-related behaviours are reported in Table 6.6. Of girls who reported an act of self-harm, every second girl reported suicidal ideation, four in ten girls reported suicide plans, and three in ten reported a suicide attempt. Out of girls who did not engage in self-harm, less than 2% reported a suicide attempt. Similar proportions were observed in boys who were engaged in self-harm (i.e., 48% of boys had suicidal ideation, 46% planned suicide, and 29% attempted suicide). Around 2% of boys who did not report self-harm reported a suicide attempt. These results indicate that 30% of young people who engage in self-harm over a 12-month period, attempt suicide.
Looking at this the other way, eight in ten girls who reported attempting suicide, reported engaging in self-harm. These proportions were significantly lower in boys who attempted suicide: one third engaged in self-harm. Thus, of those who attempted suicide, boys were less likely to engage in self-harm than girls (64% vs 20%, respectively).
Notes: Statistical significance is reported if the 95% confidence intervals do not overlap [95CI].
Source: LSAC, K cohort, Wave 6
Overall, 16% of girls (n = 249) and 7% of boys (n = 102) reported engaging in self-harm or attempting suicide.
Figure 6.1: Patterns of self-destructive behaviour, by gender
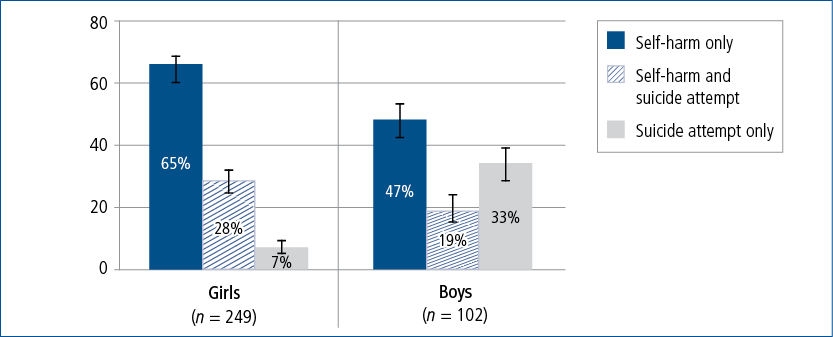
Notes: Statistical significance is reported if the 95% confidence intervals do not overlap [95CI].
Source: LSAC, K cohort, Wave 6
Figure 6.1 describes the proportion of adolescents who were engaged in either self-harm, a suicide attempt, or both. A different pattern was observed for boys and girls. Compared to boys, girls were more likely to report engaging in self-harm than boys (65% vs 47%) and less likely to report a suicide attempt only (7% vs 33%, respectively).
6.4 Factors associated with self-destructive behaviours
For better prevention and intervention strategies, it is crucial to identify factors associated with self-harm and suicidal behaviours. Rather than focusing on different types of self-destructive behaviours (thoughts of self-harm, acts of self-harm, suicidal ideation, suicide plans or attempts), this section focuses only on factors associated with acts of self-harm and suicide attempts measured as follows:
- Self-harm: There were 51 boys and 192 girls who reported engaging in self-harm within the last 12 months.
- Suicide attempt: There were 43 boys and 65 girls who reported attempting suicide at least once in the last 12 months.
For the purpose of the analysis presented in this section, only those adolescents who provided responses on all relevant variables (outcome variables and risk factors) were included (n = 2,883) and all analyses used weighted data.
List of potential risk factors
The list of potential factors associated with the increased risk of self-harm and suicide attempts was derived from the extensive literature review and included three main domains (see Introduction):
- individual factors such as adolescents' sexual development, mental and physical health, risk-taking behaviours and self-concept;
- family factors such as family's socio-economic position, financial stress, family type and child-parent relationships; and
- social relationships and school-related factors such as bullying and victimisation, sense of belonging to school and academic self-concept.
Although differences between those who engage in self-destructive behaviour (self-harm or suicidal behaviour) and others who do not can emerge in early childhood, long before adolescents engage in these behaviours, the factors that show the strongest association with such behaviours are likely to be those measured around the time that self-destructive behaviour occurs. Therefore, for the purpose of the analysis presented in this section, all the potential factors were measured at the same time as self-destructive behaviour behaviour and referred to the same time period, that is, experiences in the last 12 months. The relationships between engagement in self-destructive behaviour and early social-emotional problems as measured by the Strength and Difficulties Questionnaire (SDQ, Goodman, 2001) at earlier waves of LSAC are briefly examined in section 6.5.
All the measures used in the statistical models and how they were derived are described below.5
Individual factors
Individual factors included gender, pubertal development, temperament, sexual identity, risk-taking behaviours, mental and physical health, and general feeling of happiness.
Pubertal development was based on Puberty Category Scores developed by Crockett and Petersen (1987). The score was calculated using parents' ratings of the signs of puberty separately for boys and girls at 14 and 12 years old, respectively (for boys, body hair growth, deepening voice and facial hair growth; and for girls, body hair growth, breast development, and menarche). The score then was binarised as follows: boys with a score above 8 and girls with a score above 3 and menstruation were considered in their late or post puberty (reference category in the analysis). There were 47% of boys and 55% of girls who were in late or post puberty.
Temperament was measured using the Short Temperament Scale for Children (STSC) that comprised of three subscales: Reactivity, Persistence, and Introversion. Each scale consisted of four items with the total score being calculated as an average on the four items and the higher score reflecting a greater level of reactivity/persistence/introversion. A binary indicator for each scale was derived using quartile scores (top 25% vs the rest), with the top quartile indicating more reactive, more persistent and more introverted adolescents (reference categories).
Adolescents were asked who they were attracted to. A binary measure was derived based on adolescents' responses, that is, those who reported being attracted to the opposite gender were categorised as having heterosexual identity; those who reported being attracted to the same gender (1%), both genders (3%), being not sure to who they were attracted (3%) or reported not feeling attractions to others (4%) were categorised as having non-heterosexual identity. There were 8% of boys and 16% of girls who were categorised as having non-heterosexual identity (reference category).
Risk-taking behaviour was a composite measure derived from the following questions: "In the last 12 months have you had an alcoholic drink?"; "In the last 12 months have you had smoked/used marijuana or/and tried other drugs?"; and "Have you ever had sex?". Adolescents who reported any of these activities were considered to be involved in risky behaviour. There were around 16% of adolescents who reported risky behaviour. No gender differences were observed.
Delinquent behaviour was derived as a single indicator of involvement in crime or delinquency based on whether an adolescent had committed any of 13 violent crimes or property offences in the last 12 months. A quarter of boys and 14% of girls reported delinquent behaviour (reference category).
Their level of anxiety was derived from the Spence Anxiety Scale (short form, Spence, 1998) based on the sum of eight items. Total scores ranged from 0 to 24, with higher scores reflecting higher levels of anxiety symptoms. Boys with a total score of 9 or above and girls with a total score of 11 or above were classified as having a higher level of anxiety (reference category). There were 13% of boys and 34% of girls who reported a higher level of anxiety symptoms compared to others (reference category).
Their level of depression symptoms was derived using the Short Mood and Feelings Questionnaire (Angold, Costello, Messer, Pickles, Winder & Silver, 1995) based on the sum of 13 items. Total scores ranged from 0 to 26 with the higher scores reflecting a greater level of depression. Adolescents with scores of 8 or more were categorised as having significant depressive symptoms. There were 18% of boys and 32% of girls who were classified as having significant depressive symptoms (reference category).
Physical health was measured using PedsQL Physical Functioning scale for teens, adapted from the Pediatric Quality of Life Inventory (PedsQL) 4.0 Teen Report (ages 13-18) (Varni, 1998). The total score was calculated based on the average of eight items with the higher scores reflecting a better physical functioning. An indicator of poor physical health was derived using quartile scores (bottom 25% vs the rest), with the bottom quartile being classified as a poor level of physical health (reference category).
Adolescents were also asked whether they were generally happy with how things were for them in their life at the moment of interview. Those who were "strongly disagree"/"disagree"/"neither agree/disagree" were classified as feeling unhappy (reference category). Around a quarter of boys and a third of girls reported feeling unhappy.
Family-related factors
Family factors included family socio-demographic background (socio-economic position, residence, single-parent family, financial stress), general family wellbeing (mother's level of depression, experience of stressful life events), and parenting (difficulty monitoring, parent/child conflict, parenting styles).
Socio-economic position was calculated using a z-score based on parental occupation, education and income. An indicator of low socio-economic position (SEP) was derived using quartile scores (bottom 25% vs the rest), with those in the bottom quartile being classified as families from low socio-economic background.
Family financial stress was derived from Parent 1s' response on whether they have experienced one or more instances of financial stress in the last 12 months, as indicated by six items (e.g., parent has not been able to pay gas, electricity or telephone bills on time due to a shortage of money). Financial stress (reference category) was reported for around 15% of adolescents.
Family type was derived based on Parent 2s' presence in the home when adolescents where 14-15 years old. Around 13% of adolescents were living in the single-parent household (reference category).
Mother's level of depression was measured using the Kessler-6 (K6) scale, a six-item scale measuring psychological distress (e.g., "In the past four weeks about how often did you feel so sad that nothing could cheer you up?"). Total scores ranged from 0 to 24 with the higher scores reflecting a greater level of depression. An indicator of higher levels of depressive symptoms was derived using quartile scores (top 25% vs the rest), with the top quartile being classified as a high level of mother's depressive symptoms (reference category).
Family stressful life events were derived from parents' responses on whether any stressful life event happened to them (suffered serious illness, separation, death of a close friend/relative, etc.) in the last 12 months. Around 20% of families reported at least one stressful life event (reference category).
Time alone was measured based on adolescents' responses to how many days within the last week preceding the interview they were without an adult for an hour or more. Those who reported four or more days were classified as being alone more often (reference category). Around 24% of children reported being alone more often, there were no gender differences.
Parent 1 reported on the parent/child relationship with six items (disagree and fight, bug each other, yell at each other, stay angry, refuse to talk, stomps out of house) using a five-point scale from "1 = not at all" to "5 = all the time". The total score was derived using confirmatory factor analysis with higher scores reflecting a higher level of "fights" in the family. An indicator of a poor parent/child relationship as reported by parents was derived using quartile scores (top 25% vs the rest), with the top quartile being classified as high levels of parent/child conflict (reference category).
Parenting styles as reported by children were derived using the Parenting Style Inventory II that comprised of three scales Responsiveness, Demandingness and Autonomy-Granting (Darling & Toyokawa, 1997). Each scale consisted of five items with responses on a five-point scale from "1 = strongly agree" to "5 = strongly disagree". Total scores varied from 5 to 25 with the lower score reflecting a greater level of mother/father responsiveness/demandingness/autonomy-granting. A binary indicator of less responsive/less demanding/less autonomy-granting parenting style was derived if the respective parenting-style score at least for one parent was in the top quartile of score distribution. Among girls, 42% reported to have at least one non-responsive parent, 36% reported to have at least one non-demanding parent, and 33% reported at least one authoritative parent. Slightly smaller proportions were observed among boys, that is, 35% reported at least one non-responsive parent, 29% reported at least one non-demanding parent, and 27% reported at least one authoritative parent.
Social relationships and school-related factors
Social relationships and school-related factors included unfair treatment by peers, victimisation and bullying, communication with peers, sense of belonging to school, academic self-esteem and absenteeism.
Adolescents were asked whether they thought there were unfairly treated because of their cultural background, skin colour, language, religious belief, sexual identity/same-sex attraction, body size/shape/physical appearance, mental health problems or disability. A binary measure of whether an adolescent felt "unfairly treated" was derived if an adolescent reported "yes" to any of the above items. Around 27% of boys and 30% of girls reported feeling "unfairly treated" (reference category).
Bullying perpetration and victimisation measures were derived from the School Climate Scale (Brockenbrough et al., 2002) and the Edinburgh Study of Youth Transitions and Crime (Sweep 5, 2001), and comprised of six subscales: Physical Victimisation (three items), Verbal Victimisation (three items), Victimisation by Isolation (two items), Physical Perpetration (three items), Verbal Perpetration (three items), and Perpetration by Isolation (two items). For each scale a binary indicator was derived for those who reported at least one experience in the last 12 months (reference category). Around 40% of boys and 23% of girls reported being physically victimised (e.g., being hit or kicked, being grabbed or shoved); around 45% of boys and girls reported being verbally victimised (e.g., were threatened to be hurt or were called mean things); and 26% of boys and 42% of girls reported being deliberately isolated from peers (e.g., were not let to join in). Around 29% of boys and 10% of girls reported bullying others physically (e.g., hit or kicked, grabbed or shoved); 29% of boys and 20% of girls reported threating others (e.g., threatened to hurt or called others mean things); and about 13% of boys and girls reported deliberately isolating others (e.g., did not let others join in).
Sense of belonging to school was measured using the Psychological Sense of School Membership (short form) that consisted of 12 items. The total score was calculated as the mean of the 12 items with higher scores reflecting a stronger sense of belonging to school. A binary indicator was derived using quartile scores (bottom 25% vs the rest), with the bottom quartile indicating adolescents with a weak sense of belonging to school (reference category).
The frequency of unauthorised absences from school was measured using adolescents' reports on a number of times the adolescent was absent from school without parental permission during the last two weeks preceding the interview. A binary indicator was derived to identify adolescents who had any unauthorised absences during this period (reference category). Around 5% of adolescents were absent from school without parental consent during two weeks preceding the interview. There were no gender differences.
Analytical approach
To identify the risk factors associated with adolescents' engagement in self-harm, logistic regressions were estimated with results reported as an odds ratio.6 The odds ratio (OR) is a relative measure of risk, which tells how much more likely it is that someone who is exposed to the factor under study will develop the outcome compared to someone who is not exposed. The OR of greater than 1 suggests that the self-harm is more likely for those who were exposed to the factor compared to those who were not. The odds ratio of 1 suggests that there is no difference in the likelihood of self-harm between two groups. An OR of less than 1 suggests that self-harm is less likely for those who were exposed to the factor compared to those who were not.
In order to identify the main factors associated with self-harm, four models were estimated:7
- Model 1: includes individual variables only. This model allows examination of the association between adolescent's characteristics and self-harm, in the absence of any other contributing factors.
- Model 2: includes family variables only. This model allows an evaluation of the unique contribution of family factors independent of child and school and friends factors.
- Model 3: includes school and social relationships variables only. This model assesses the role of school characteristics and social relations independently of other factors.
- Model 4: includes all of the above variables. This model allows us to determine the most significant factors associated with self-harm.
To ensure that the differences across models are not attributed to differences in sample size due to missing data on various variables, only those adolescents who provided data on all variables of interest across four models were included in the analysis (i.e., complete case analysis). As a result, the sample size was 2,883 individuals. Gender differences were tested using interaction effects.
A similar approach was employed to identify factors associated with a suicide attempt. As the majority of young adolescents who attempted suicide were also likely to engage in self-harm and girls were more likely to engage in self-harm, it was important to identify the unique contribution of different factors after accounting for self-harm and gender. The sample size was 2,882 individuals. Gender differences were tested using interaction effects.
Risk factors associated with self-harm
Table 6.7 presents results for logistic regressions of self-harm, focusing on different factors in separate multivariate regressions within blocks (individual variables, family and parenting variables, school and peer-related variables), and then entered into the final model.
Across all models, females were more likely to self-harm than boys. When only individual characteristics were considered (Model 1), adolescents were at a greater risk of engaging in self-harm behaviour if they reported:
- being attracted to adolescents of the same gender, or both genders, or not being attracted to anyone (OR = 1.91, p < 0.01);
- a higher level of temperamental reactivity (OR = 2.01, p < 0.001);
- being engaged in risky behaviour in the last 12 months (OR = 2.32, p < 0.001);
- delinquent behaviour (OR = 1.56, p < 0.01);
- having symptoms of depression (OR = 7.26, p < 0.001);
- having symptoms of anxiety, though gender differences were observed. Among adolescents who did not report anxiety symptoms, girls were more likely to engage in self-harm compared to boys; and
- being generally not happy at the time of the interview (OR = 2.35, p < 0.001).
Physical health, early pubertal development and other temperament characteristics were not associated with an increased risk of self-harm. All these factors but engagement in delinquent behaviour remained statistically significant even after controlling for family, parenting, peer and school characteristics.
When only family characteristics were considered (Model 2), the factors associated with an increased risk of self-harm were:
- non-responsive parent as reported by adolescent (OR = 2.31, p < 0.001);
- more authoritative parent as reported by adolescent (OR=2.31, p < 0.01); and
- conflict between parents and adolescent as reported by parent (OR = 1.63, p < 0.001).
Socio-demographic characteristics, such as family socio-economic position, experience of financial stress, and type of household as well as other family characteristics such as stressful events and difficulty monitoring were not associated with an increased risk of self-harm. No gender differences were observed. When we controlled for child, parenting and school characteristics, parenting characteristics and family-related factors were no longer associated with a greater risk of self-harm.
In Model 3, when school-related characteristics and peer relationships were examined, adolescents were at a greater risk of engaging in self-harm behaviour if they reported:
- being treated unfairly by their peers (OR = 2.47, p < 0.001);
- being kicked/hit/shoved/grabbed in the last 12 months (OR = 1.58, p < 0.05);
- being verbally threatened by their peers, though only for girls;
- poor school belonging (OR = 2.70, p < 0.001); and
- being frequently absent from school (OR = 2.97, p < 0.001).
Being a bully was not associated with an increased risk of self-harm when we controlled for other factors within the social domain. In the full model (Model 4), adolescents who reported being unfairly treated or verbally threated by their peers were at an increased risk of self-harm.
Notes: Statistically significant differences are noted: * p < .05; ** p < .01; *** p < .001.
The results of the final model (Model 4) suggest that individual characteristics and relationships with peers are the main factors associated with an increased risk of self-harm. Overall, girls were more likely to engage in self-harm behaviour than boys; however, some differences were apparent. Boys who reported anxiety symptoms were more likely to self-harm compared to boys with no anxiety symptoms. There were no differences observed among girls by anxiety level (Figure 6.2). Among adolescents who reported being verbally threatened by others, girls were more likely than boys to report self-harm (Figure 6.2).
Also, the odds of self-harm were greater among adolescents:
- who reported being attracted to other adolescents of the same sex, both sexes or not being attracted to anyone compared to those who reported being attracted only to the opposite sex (OR = 1.89, p < 0.001);
- with a more reactive temperament compared to those who were less reactive (OR = 1.68,
p < 0.05); - who reported having depression compared to those who did not show any depressive symptoms (OR = 6.40, p < 0.001);
- who reported feeling not happy compared to those who generally felt happy with their life (OR = 2.15, p < 0.001); and
- who reported being treated unfairly by their peers because of their health, skin colour, sexual orientation, language, culture or religion compared to those who felt they were being treated fairly (OR = 1.71, p < 0.05).
Figure 6.2: Adjusted probabilities of self-harm by anxiety symptoms and peer victimisation (verbal threatening) and gender
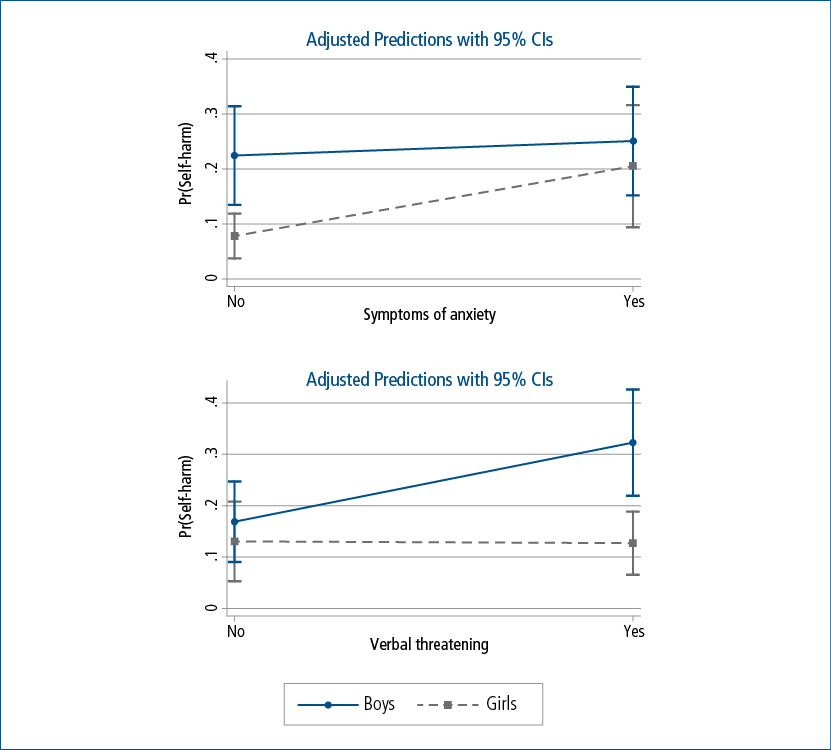
Note: Predicted probabilities are calculated after adjusting for all other variables shown in Model 4, in Table 6.7.
Risk factors of suicide attempt
Table 6.8 presents results for logistic regressions of suicide, focusing on individual factors within each block (individual factors, family demographics and parenting, school and peers) in separate multivariate regressions, and then all blocks in the final model.
In all four models presented below, we have controlled for self-harm for two main reasons. Firstly, previous research suggests that adolescents' engagement in self-harm is a significant risk factor for suicide attempts. In the current sample, the odds of a suicide attempt were 20 times greater among adolescents who reported self-harm than those who did not (OR = 20.46, p < 0.001). Secondly, risk factors associated with suicide-related behaviours are similar to the risks factors associated with self-harm (Prinstein, 2008).
When only individual characteristics were considered (Model 1), adolescents were at a greater risk of a suicide attempt if they reported:
- engagement in self-harm behaviour (OR = 9.32, p < 0.001);
- being attracted to adolescents of the same gender, or both genders, or not being attracted to anyone (OR = 2.10, p < 0.01);
- being involved in any crime or property offences in the last 12 months (OR = 1.89, p < 0.01); and
- being generally not happy (OR = 1.88, p < 0.05).
There were no gender differences observed. When all the factors across three domains were included in the final model, only adolescents' sexual identity and delinquent behaviour were associated with a risk of suicide attempts.
Notes: Statistically significant differences are noted: * p < .05; ** p < .01; *** p < .001.
In Model 2, the odds of a suicide attempt were greater among adolescents who reported self-harm compared to those who did not (OR = 16.55, p < 0.001); adolescents with mothers with depressive symptoms compared to those with mothers with no signs of depression (OR = 1.75, p < 0.05); and adolescents with at least one very authoritative parent compared to those who had less authoritative parents (OR = 1.83, p < 0.01). Other family and parenting factors were not associated with a suicide attempt, nor were there any gender differences observed. In the final model, after controlling for child, school and peer characteristics, family factors were not associated with an increased risk of suicide attempts.
In Model 3, when school-related characteristics and peer relationships were examined, adolescents were at a greater risk of a suicide attempt if they reported self-harm behaviour in the last 12 months (OR = 13.37, p < 0.001) and a poor sense of belonging to school (OR = 1.99, p < 0.01). There were no gender differences observed. Factors such as bullying, victimisation, school absenteeism, negative academic self-esteem and poor communication with peers were not associated with an increased risk of a suicide attempt. In the final model, school-related characteristics and relationships with peers were not associated with suicide attempt.
The results of the final model (Model 4) suggest that, after controlling for self-harm and all other child, family and school characteristics as well as relationship with peers, the only factors associated with an increased risk of a suicide attempt were engagement in self-harm, an adolescent's sexual identity and delinquent behaviour. The odds of a suicide attempt were greater among adolescents:
- who reported engagement in self-harm behaviour in the last 12 months compared to those who did not report self-harm (OR = 9.18, p < 0.001);
- who reported being attracted to the same sex or both sexes, not being attracted to anyone or not knowing who they were attracted to compared to those who reported being attracted only to the opposite sex (OR = 2.05, p < 0.05);
- who reported being involved in any crime or property offences in the last 12 months compared to those who did not engage in any delinquent behaviour (OR=1.81, p < 0.05).
6.5 Co-variation with early indicators of mental health
In the previous section the focus was on understanding the relationship between self-destructive behaviour and factors that were measured around the time the self-harm or suicide attempt occurred, that is, from the Wave 6 LSAC interview. But the predisposition to engage in self-harm and/or attempt suicide can emerge in early childhood, long before adolescents engage in these behaviours. Research suggests that poor socio-emotional wellbeing and mental health problems could be early indicators identifying those at a greater risk of engagement in self-harm and/or attempted suicide (Chapman, Gratz, & Brown, 2006; Esposito-Smythers, et al., 2010). Therefore, this section examines how many adolescents who reported self-destructive behaviour at 14-15 years of age already showed signs of socio-emotional problems at 10-11 or 12-13 years of age.
Early indicators of mental health
Indicators of mental health were derived from children's reports on socio-emotional problems based on the Strength and Difficulties Questionnaire (Goodman, 2001). This instrument is a brief screening tool that includes four scales assessing conduct problems, emotional problems, hyperactivity and peer problems. Each scale measures the degree of reported problems a child may be experiencing and comprises five items with response options from 0 to 10. Higher scores indicate higher levels of socio-emotional problems. The total "difficulty" score is aggregated from responses to questions from these four scales. In this analysis, children's reports at 10-11 and 12-13 years of age were used. To identify children with relatively high problems at multiple ages, a longitudinal measure was derived. Firstly, at each age, children in the bottom 33% of the distribution of each scale were distinguished from the remainder of children. Then, a longitudinal measure with two categories was derived for each scale and the total score:
- never had relatively high problems (non-elevated level); and
- had relatively high problems at 10-11 or/and 12-13 years old (elevated level).
The chi-square tests were used to compare proportions of young people who engaged in self-harm and made a suicide attempt by earlier indicators of their socio-emotional wellbeing.
Risk of self-harm by early indicators of mental health
Engagement in self-destructive behaviour (self-harm and suicide attempts) was strongly associated with socio-emotional problems identified at earlier ages (Figure 6.3). Almost half of the adolescents who reported self-harm at 14-15 years had the following problems at 10-11 and 12-13 years of age: conduct problems (49%), peer problems (43%), emotional problems (51%) and hyperactivity (43%). Among adolescents who did not report self-harm, the proportion of adolescents with socio-emotional problems was smaller, that is, 29% of these adolescents had conduct problems, 26% had peer problems, 31% emotional problems and 29% hyperactivity problems. Differences were also observed in the total problems score. Among adolescents who did self-harm, 56% had high levels of total problems at early ages compared to 30% among those who did not self-harm. No gender differences were observed.
A similar tendency was observed for suicidal behaviour. Among those who attempted suicide, a greater proportion of adolescents had socio-emotional problems in early or pre-teen years: 65% had conduct problems, 52% had peer problems, 55% had emotional problems and 46% had hyperactivity problems. There were no gender differences observed.
It is important to emphasise that among the 14-15 year olds who did report self-destructive behaviour, a large proportion did not have any socio-emotional problems in their pre-teen (10-11 years old) and early teen (12-13 years old) years.
We also examined whether early internalising problems were risk factors of self-destructive behaviour, above and beyond adolescents' current mental health symptoms. Table 6.9 reports odds ratios of self-harm and suicide attempts among adolescents who had socio-emotional problems at early and/or pre-teen years and those who had not, controlling for all other risk factors measured at the same time as self-harm or a suicide attempt occurred. Two different models were fitted:
Figure 6.3: Self-destructive behaviour at 14-15 years old by internalising problems at 10-11 and/or 12-13 years old
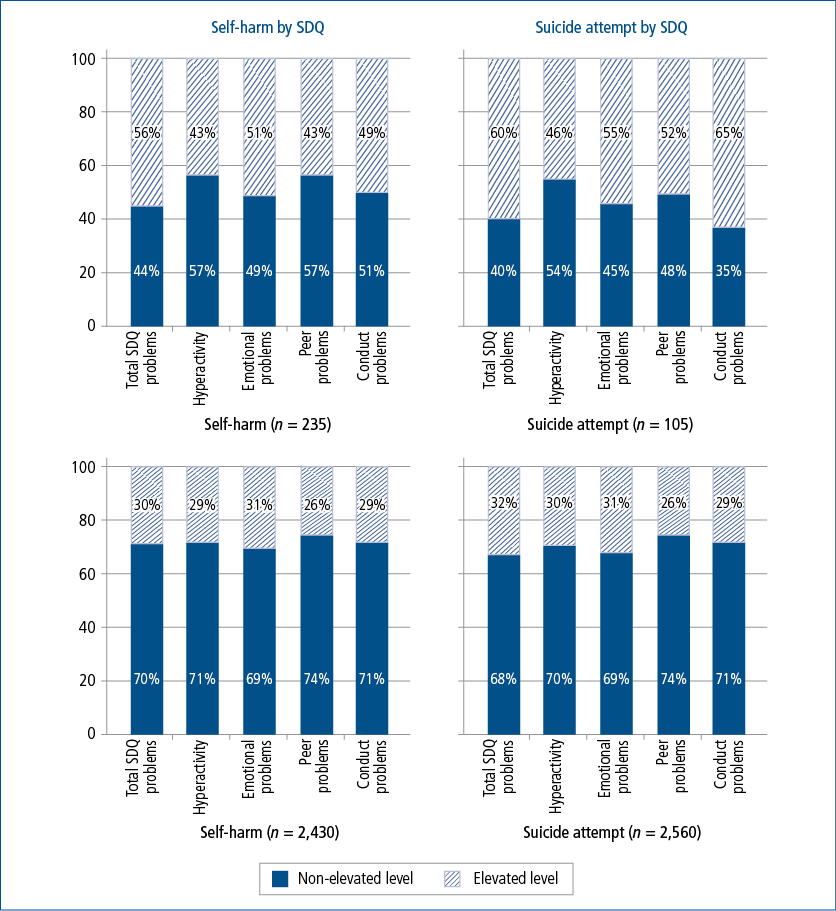
Notes: Statistical significance was examined using chi-square test. All the differences were statistically significant at: p < .001. Weighted sample.
Source: LSAC, K cohort, Waves 4, 5 & 6
- Model 1 - SDQ Scales: incudes four measures of adolescents' early mental health symptoms derived from the SDQ subscales and their current symptoms of mental health derived from the Short Mood and Feelings Questionnaire and Spence anxiety scale controlling for individual characteristics, family and parenting characteristics, school characteristics and relationships with peers.
- Model 2 - SDQ Total: includes one measure of adolescents' early mental health symptoms derived from the SDQ total score and their current symptoms of mental health derived from the Short Mood and Feelings Questionnaire and Spence anxiety scale controlling for individual characteristics, family and parenting characteristics, school characteristics and relationships with peers.
There were no significant associations between self-harm and early symptoms of poor mental health after controlling for individual characteristics, family and parenting characteristics, school characteristics and relationships with peers. But the odds of a suicide attempt were greater among adolescents who had higher scores on the SDQ Conduct Problems scale at 10-13 years of age compared to those who did not, even after controlling for adolescents' engagement in self-harm, concurrent mental health problems, and other individual, family and social characteristics.
Notes: Statistically significant differences are noted: * p < .05; ** p < .01; *** p < .001. Weighted sample. a Controls: female, non-heterosexual identity, early pubertal development, persistence, reactivity, introversion, risky behaviour, delinquent behaviour, poor physical health, unhappiness, low SEP, financial stress, single-mum household, stressful family events, difficulty monitoring, often alone, mum's depression, non-responsive parent, non-demanding parent, authoritative parent, child-parent conflict, unfair treatment, physical victimisation, verbal threatening, isolation by peers, physical bully, verbal bully, isolation bully, poor belonging to school, frequently absent. b Controls: self-harm, female, non-heterosexual identity, early pubertal development, persistence, reactivity, introversion, risky behaviour, delinquent behaviour, poor physical health, unhappiness, low SEP, financial stress, single-mum household, stressful family events, difficulty monitoring, often alone, mum's depression, non-responsive parent, non-demanding parent, authoritative parent, child-parent conflict, unfair treatment, physical victimisation, verbal threatening, isolation by peers, physical bully, verbal bully, isolation bully, poor belonging to school, frequently absent.
Source: LSAC, K cohort, Waves 4, 5 & 6
6.6 Conclusion and key implications
Self-harm and suicide-related behaviour accounts for a considerable portion of disability burden and mortality among adolescents, yet the majority of incidents of such behaviour do not come to the attention of health services or even parents and friends. The purpose of this report was to establish the 12-month prevalence of self-harm and suicide-related behaviours among 14-15 year olds and identify key risk factors associated with such behaviours.
Prevalence rates
Using nationally representative data for 14-15 year olds born in 1999/2000, it was estimated that 15% of girls and 4% of boys reported engaging in self-harm in the last 12 months. Among girls, 12% reported suicidal ideation, 9% developed a suicide plan, and 6% attempted suicide. Smaller rates were reported in boys: 6% of boys experienced suicidal ideation, 5% developed a plan, and 4% attempted suicide. These estimates were higher than the ones reported for 12-15 years old and similar to the ones reported for 16-17 years old in the second Child and Adolescent Survey of Mental Health and Wellbeing (Lawrence et al., 2015). The differences are mainly attributed to differences in the reference group. In the current research, the estimates were presented for 14-15 year olds, whereas in the Mental Health study, the estimates were presented for 12-15 year olds and 16-17 year olds, not for 14-15 years old separately. As 12-13 year olds are less likely to engage in self-harm and suicidal behaviour is comparatively uncommon in the younger age group, the prevalence rates of 12-15 year olds reported in the Child and Adolescent Survey of Mental Health and Wellbeing would have been lower when reporting on the broader age range.
This research aimed to examine the pathways of suicide attempts. Only one third of adolescents with suicidal ideation did not report any other suicide-related behaviours, whereas approximately half of adolescents with suicidal ideation reported developing a suicide plan and one third (three in ten boys and four in ten girls) reported a suicide attempt. Among those who attempted suicide, six in ten adolescents reported a suicide plan at some point in the last 12 months, suggesting that at least 40% of suicide attempts were unplanned, with the proportion of unplanned suicide attempts being greater among boys than girls (58% of boys and 31% of girls). This finding is consistent with previous research that has shown that impulsive suicide attempts are more common among males than females (Simon et al., 2001). When monitoring youth at risk of attempting suicide, it is important to also be aware of the risk factors that may help to identify those who are more likely to attempt an unplanned suicide (most likely out of impulsiveness).
Important relationships were also observed between self-harm and suicide attempts. Among those who engaged in either of these forms of self-destructive behaviour, one third of boys and girls reported a suicide attempt, whereas among those who attempted suicide, a greater proportion of girls (79%) than boys (36%) reported engaging in self-harm, highlighting the elevated risk of attempted suicide in girls who have self-harmed. In contrast, among those who did not engage in self-harm, boys were more likely to report attempting suicide than girls (33% vs 7%). These findings are consistent with previous research and highlight gender differences in the pathways of self-harm and may reflect different patterns and psychological functions of self-harm between boys and girls that need to be taken into account in developing prevention programs (Andover et al., 2010; Whitlock et al., 2011; Nock, Green, Hwang, McLaughlin, Sampson, Zaslavsky, Kessler, 2013).
While there is no "causal" order in suicidal ideation, plans and attempts, this phenomenology provides an important insight into possible pathways of suicidal behaviour. In addition, these findings are important not only for the scientific understanding of suicidal behaviour but also for developing preventive strategies.
Risk factors
This chapter also provided further insights around risk factors of self-harm and suicide attempts and examined whether there were gender differences. Consistent with previous research, a large number of factors were associated with an increased risk of self-harm: adolescents' risky behaviours (Madge et al., 2011; Aseltine et al., 2009), temperament, victimisation and discrimination (Bureau et al., 2010; Prinstein et al., 2010; Jarvi et al., 2013), non-heterosexual identity (Ryan et al., 2009), high levels of depression and anxiety (Haw et al., 2001; Skegg, 2005), parenting styles and child-parent conflict (Fergusson et al., 2007; Brent & Mann, 2005), a general feeling of unhappiness, and poor sense of belonging to school (Kidger et al., 2015).
However, after controlling for all cofounders, individual characteristics and experience of peer victimisation were the only key risk factors associated with an increased risk of self-harm. That is, the odds of engagement in self-harm were significantly greater among females compared to males; adolescents who reported being attracted to the same sex, both sexes, or were not sure who they attracted to compared to those who were attracted to the opposite sex only; adolescents with a reactive temperament compared to those without; adolescents with depressive and anxiety symptoms compared to non-depressive and non-anxious adolescents; adolescents who engaged in any risky behaviour (substance abuse, drinking, or sexual activity) compared to those who did not; adolescents who did not feel generally happy compared to those who did; adolescents who reported being unfairly treated because of their race, religion, skin colour, look, disability, etc. compared to those who did not.
While both boys and girls with anxiety symptoms were likely to self-harm, among those without anxiety symptoms, girls were more likely to self-harm than boys. Gender differences were also observed in the experiences of peer victimisation. Among adolescents who reported being verbally threatened by others, girls were more likely to report self-harm compared to boys.
A broad range of factors that were associated with self-harm were also risk factors for attempting suicide. Once engagement in self-harm was taken into account, a number of factors were no longer associated with elevated odds of attempting suicide. The key factors that did remain significant were engagement in self-harm, non-heterosexual identify and delinquent behaviour. The results suggest that even though not every adolescent who engages in self-harm proceeds with a suicide attempt, self-harm serves as a "gateway" for suicide attempt (Whitlock, et al., 2013). Therefore, there is a need for early response and intervention on any act of self-harm. For example, screening for self-harm may aid in the identification of adolescents at risk of attempting suicide.
This chapter has also explored the potential association between the risk of self-harm and attempted suicide and early indicators of adolescents' mental health measured two and four years prior to reporting an act of self-harm and/or attempted suicide. In line with previous research, the results signify the important relationships between socio-emotional problems experienced in early and pre-teen years and elevated risks of self-harm and suicide attempts for young people (Hintikka et al., 2009). These findings suggest that screening using early indicators of mental health may assist greatly in identifying those at a greater risk of self-destructive behaviour, particularly self-harm. However, relying only on screening would lead to missing a substantial proportion of young people who do engage in self-harm and attempt suicide but have not experienced these problems during the four years prior to their self-harming.
Overall, the findings highlight that interventions and preventive strategies should take place at both individual and school levels. These preventative strategies should be directed towards young people, in order to increase their awareness of risk factors for themselves and also their peers, as well as increase awareness of the support services and other resources available (e.g., Lifeline, beyondblue, local support groups or online resources such as MindSpot or ECouch), which can be a starting point for identifying issues and finding support. Programs to assist teachers and parents to appropriately assess the signs of self-harm and suicidal intent, including identifying those who are more likely to attempt suicide unplanned (most likely out of impulsiveness), could be of considerable benefit for reducing the overall disability burden of self-destructive behaviour of young people.
Limitations
These findings should be interpreted in light of several limitations, though. First, there were not many gender differences identified. This might be due to low statistical power for tests of interaction effects, especially when controlling for a number of cofounders. Secondly, while the study included measures of mental health, anxiety and depression, specific mental disorders (both ongoing and clinically diagnosed) known to be associated with self-harm and suicidal behaviour, identified early in the child's life were not included in the analysis. It would be of great importance to understand, using longitudinal data, causal pathways linking child-adolescent mental disorders to adolescents' self-harm and suicidal behaviour. The insights will be not only of scientific value but also assist in developing actionable strategies of clinical prediction and prevention of these behaviours. Lastly, the temporal relationship between self-harm and suicide attempts was not taken into account. It was assumed that self-harm behaviour was preceding or concurrent to a suicide attempt. Understanding why young people change course could provide important insights into how to prevent suicidal behaviours and suicide itself. Therefore, examining temporal relationships between self-harm and suicide attempts and understanding mechanisms that trigger adolescents to end their life would be important research in its own right. These limitations notwithstanding, the chapter provides valuable information about self-harm and the suicide-related behaviour of 14-15 year olds and emphasises a need for timely and targeted interventions.
6.7 References
Angold, A., Costello, E. J., Messer, S. C., Pickles, A., Winder, F., & Silver, D. (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237-249.
Aseltine, R. H., Schilling, E. A., James, A., Glanovsky, J. L., & Jacobs, D. (2009). Age variability in the association between heavy episodic drinking and adolescent suicide attempts: Findings from a large-scale, school-based screening program. Journal of the American Academy of Child and Adolescent Psychiatry, 48(3), 262-270.
Australian Bureau of Statistics (ABS). (2007). National Survey of Mental Health & Wellbeing. Canberra: ABS.
Australian Bureau of Statistics (ABS). (2016). Causes of death, Australia, 2014 (3303.0). Canberra: ABS. Retrieved from <www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0~2014~Main%20Features~Key%20Characteristics~10054>.
AVON Longitudinal Study of Parents and Children (ALSPAC). (2007). Life of a 16+ teenager questionnaire. Bristol: ALSPAC, University of Bristol.
Baetens, I., Claes, L., Onghena, P., Muehlenkamp, J., & Grietens, H. (2011). Non-suicidal and suicidal self- injurious behavior among Flemish adolescents: A web survey. Archives of Suicide Research, 15(1), 56-67.
Bergen, H., Hawton, K., Waters, K., Ness, J., Cooper, J., Steeg, S., & Kapur, N. (2012). Premature death following self-harm: A multicentre cohort study. The Lancet, 380(9853), 1568-1574.
Brent, D. A., & Mann, J. J. (2005). Family genetic studies, suicide, and suicidal behaviour. American Journal of Medical Genetics. Part C, Seminars in medical genetics, 133C(1), 13-24.
Brockenbrough, K. K., Cornell, D. G., & Loper, A. B. (2002). Aggressive attitudes among victims of violence at school. Education and Treatment of Children, 25, 273-287.
Bureau, J. F., Martin, J., Freynet, N., Poirier, A. A., Lafontaine, M. F., & Cloutier, P. (2010). Perceived dimensions of parenting and non-suicidal self-injury in young adults. J Youth Adolesc, 39(5), 484-494. doi: 10.1007/s10964-009-9470-4
Cash, S. J., & Bridge, J. A. (2009). Epidemiology of youth suicide and suicidal behavior. Current Opinion in Pediatrics, 21(5), 613-619.
Chapman, A. L., Gratz, K. L., & Brown, M. Z. (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy, 44(3), 371-394.
Conner, K. R., Langley, J., Tomaszewski, K. J., & Conwell, Y. (2003). Injury hospitalization and risks for subsequent self-injury and suicide: A national study from New Zealand. American Journal of Public Health, 93(7), 1128-1131.
Crockett, L. J., & Petersen, A. C. (1987). Pubertal status and psychosocial development: Findings from the early adolescence study (Faculty Publications, Department of Psychology, Paper 227). Lincoln: University of Nebraska.
Darling, N., & Toyokawa, T. (1997). Construction and validation of the parenting style inventory II (PSI-II). Unpublished manuscript.
Esposito-Smythers, C., Spirito, A., Hunt, J., Kahler, C., & Monti, P. (2010). Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized pilot trial. Manuscript submitted for publication. [PMC free article] [PubMed].
Evans, E., Hawton, K., & Rodham, K. (2004) Factors associated with suicidal phenomena in adolescents: A systematic review of population-based studies. Clinical Psychology Review, 24(8), 957-979.
Fergusson, D. M., Boden, J. M., & Horwood, L. J. (2007). Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. The British Journal of Psyhiatry, 191(4), 335-342.
Fergusson, D. M., Boden, J. M., & Horwood, L. J. (2008). Exposure to childhood sexual and physical abuse and adjustment in early childhood. Child Abuse & Neglect, 32(6), 607-619.
Fisher, H., Moffitt, T., Houts, R., Belsky, D., Arseneault, L., & Caspi, A. (2012). Bullying victimisation and risk of self-harm in early adolescence: Longitudinal cohort study. BMJ, 2012(344), e2683
Fortune, S., Stewart, A., Yadav, V., & Hawton, K. (2007). Suicide in adolescents: Using life charts to understand the suicidal process. Journal of Affective Disorders, 100(supplement 1), S1-S64.
Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581-586.
Gore, F. M., Bloem, P. J., Patton, G. C., Ferguson, J., Joseph, V., & Coffey, C., et al. (2011). Global burden of disease in young people aged 10-24 years: A systematic analysis. The Lancet, 377(9783), 2093-2102. doi: 10.1016/S0140-6736(11)60512-6
Gosney, H., & Hawton, K. (2007). Inquest verdicts: Youth suicides lost. Psychiatric Bulletin, 31, 230-205.
Haq, S., Subramanyam, D., & Agius, M. (2010). Assessment of self-harm in an accident and emergency service: The development of a proforma to assess suicide intent and mental state in those presenting to the emergency department with self-harm. Psychiatr Danub, 22(Suppl 1), S26-32.
Haw, C., Hawton, K., Houston, K., & Townsend, E. (2001) Psychiatric and personality disorders in deliberate self-harm patients. British Journal of Psychiatry, 178(1), 48-54.
Hawton, K., & James, A. (2005). Suicide and deliberate self harm in young people. BMJ, 330(7496), 891-894.
Hawton, K., Saunders, K., & O'Connor, R. (2012). Self-harm and suicide in adolescents. The Lancet, 379(9834), 2373-2382.
Hintikka, J., Tolmunen, T., Rissanen, M. L., Honkalampi, K., Kylma, J., & Laukkanen, E. (2009). Mental disorders in self-cutting adolescents. Journal of Adolescent Health. doi:10.1016/j.jadohealth.2008.10.003, 2009
Houston, K., Hawton, K., & Shepperd, R. (2001). Suicide in young people aged 15-24: A psychological autopsy study. Journal of Affective Disorders, 63(1-3), 159-170.
Jacobson, C. M., & Gould, M. (2007). The epidemiology and phenomenology of non-suicidal self-injurious behavior among adolescents: A critical review of the literature. Archives of Suicide Research, 11, 129-147.
Jarvi, S., Jackson, B., Swenson, L., & Crawford, H. (2013). The impact of social contagion on non-suicidal self-injury: A review of the literature. Archives of Suicide Research, 17(1), 1-19.
Kidger, J., Heron, J., Leon, D., Tilling, K., Lewis, G., & Gunnella, D. (2015). Self-reported school experience as a predictor of self-harm during adolescence: A prospective cohort study in the South West of England (ALSPAC). Journal of Affective Disorders, Mar 1, 163-169.
King, M., Semlyen, J., See Tai, S., Killaspy, H., Osborn, D., Popelyuk, D., & Nazareth, I. (2008). A systematic review of mental disorder, suicide and deliberate self-harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(70).
Klomek, A. B., Sourander, A., Niemelä, S., Kumpulainen, K., Tamminen, T., Almqvist, F., & Gould, M. S. (2009). Childhood bullying behaviours as a risk for suicide attempts and completed suicides: A population-based birth cohort study. Journal of the American Academy of Child & Adolescent Psychiatry, 48(3), 254-261.
Klonsky, E. D. (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27(2), 226-239.
Klonsky, E. D., & Muehlenkamp, J. (2007). Self-injury: A research review for the practitioner. Journal of Clinical Psychology, 63(11), 1045-1056.
Kumar, G., Pepe, D., & Steer, R. A. (2004). Adolescent psychiatric inpatients' self-reported reasons for cutting themselves. Journal of Nervous and Mental Disease, 192(12), 830-836.
Lang, C. M., & Sharma-Patel, K. (2011). The relation between childhood maltreatment and self-injury: A review of the literature on conceptualization and intervention. Trauma, Violence & Abuse, 12(1), 23-37.
Lawrence, D., Johnson, S., Hafekost, J., Boterhoven De Haan, K., Sawyer, M., Ainley, J., & Zubrick, S. (2015). The mental health of children and adolescents (Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing). Canberra: Department of Health.
Madge, N., Hawton, K., McMahon, E. M., Corcoran, P., De Leo, D., de Wilde, E. J. et al. (2011). Psychological characteristics, stressful life events and deliberate self-harm: Findings from the Child and Adolescent Self-harm in Europe (CASE) Study. European Child & Adolescent Psychiatry, 20(10), 499-508.
Madge, N., Hewitt, A., Hawton, K., Jan de Wilde, E., Corcoran, P., Fekete, S., et al. (2008). Deliberate self-harm within an international community sample of young people: Comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. Journal of Child Psychology and Psychiatry, 49(6), 667-677.
Maniglio, R. (2011). The role of child sexual abuse in the etiology of substance-related disorders. Journal of Addictive Diseases, 30(3), 216-228. doi: 10.1080/10550887.2011.581987
Martin, G., Swannell, S., Harrison, J., Hazell, P., & Taylor, A. (2009). The Australian National Epidemiological Study of Self-injury (ANESSI). Brisbane: Centre for Suicide Prevention Studies.
McMahon, E., Keeley, H., Cannon, M., Arensman, E., Perry, I. J., Clarke, M. et al. (2014). The iceberg of suicide and self-harm in Irish adolescents: A population-based study. Social Psychiatry and Psychiatric Epidemiology, 49(12), 1929-1935.
Meltzer, H., Lader, D., Corbin, T., Singleton, N., Jenkins, R., & Brugha, T. (2002) Non-Fatal Suicidal Behaviour Among Adults aged 16 to 74 in Great Britain. London: The Stationery Office.
Moran, P. , Coffey, C., Romaniuk, H., Olsson, C., Borschmann, R., Carlin, J. B., & Patton, G. C. (2012). The natural history of self-harm from adolescence to young adulthood: A population-based cohort study. The Lancet, 379(9812), 236-243.
Muehlenkamp, J., Claes, L., Havertape, L., & Plener, P. (2012). International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child and Adolescent Psychiatry and Mental Health, 6(10), 1753-2000.
Muehlenkamp, J., & Gutierrez, P. M. (2004). An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-Threatening Behavior, 34(1), 12-23.
Muehlenkamp, J., & Gutierrez, P. M. (2007). Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Archives of Suicide Research, 11(1), 69-82.
Nixon, M. K., Cloutier, P. F., & Aggarwal, S. (2002). Affect regulation and addictive aspects of repetitive self-injury in hospitalized adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 41(11), 1333-1341.
Nock, M. K., Greif Green, J., Hwang, I., McLaughlin, K. A., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Prevalence, correlates and treatment of lifetime suicidal behavior among adolescents. JAMA Psychiatry, 70(3), 300-310.
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885-890.
Patton, G. C., Hemphill, S. A., Beyers, J. M., Bond, L., Toumbourou, J. W., McMorris, B. J., & Catalano, R. F. (2007). Pubertal stage and deliberate self-harm in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 46(4), 508-514.
Plener, P. L., Schumacher, T. S., Munz, L. M., & Groschwitz, R. C. (2015). The longitudinal course of non-suicidal self-injury and deliberate self-harm: A systematic review of the literature. Borderline Personality Disorder and Emotion Dysregulation, 2(2).
Prinstein, M. J., Heilbron, N., Guerry, J. D., Franklin, J. C., Rancort, D., Simon, V. et al. (2010). Peer influence and nonsuicidal self-injury: Longitudinal results in community and clinically-referred adolescent samples. Journal of Abnormal Child Psychology, 38, 669-682.
Prinstein, M. J., Nock, M. K., Simon, V., Aikin, J. W., Cheah, C. S. L., & Spirito, A. (2008). Longitudinal trajectories and predictors of suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology, 76, 92-103.
Reinherz, H. Z., Giaconia, R. M., Silverman, A. B., Friedman, A., Pakiz, B., Frost, A. K., & Cohen, E. Early psychosocial risks for adolescent suicidal ideation and attempts. Journal of the American Academy of Child and Adolescent Psychiatry, 34(5), 599-611.
Ross, S., Heath, N. L., & Toste, J. R. (2009) Non-suicidal self-injury and eating pathology in high school students. American Journal of Orthopsychiatry, 79(1), 83-92.
Royal Australian and New Zealand College of Psychiatrists. (2009). Self-harm: Australian treatment guide for consumers and carers. Melbourne: The Royal Australian and New Zealand College of Psychiatrists.
Ryan, C., Huebner, D., Diaz, R. M., & Sanchez, J. (2009). Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics, 123(1), 346-352.
Simon, T. R., Swann, A. C., Powell, K. E., Potter, L. B., Kresnow, M. J., & O'Carroll, P. W. (2001), Characteristics of Impulsive Suicide Attempys and Attempters, Suicide and Life Threatening Behaviour, 32, 49-59.
Skegg, K. (2005) Self-harm. Lancet, 366(9495), 1471-1483.
Spence, S. (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36(5), 545-566.
Varni, J. W., Seid, M., Rode, C. A. (1999). The PedsQL: Measurement model for the pediatric quality of life inventory. Med Care; 37(2), 126-139.
Warren, D., & Yu, M. (2016). Pubertal status and emotional, school and social functioning. In Australian Institute of Family Studies (Ed.), LSAC Annual Statistical Report 2015 (pp. 127-151). Melbourne: AIFS.
Whitlock, J., Muehlenkamp, J., Eckenrode, J., Purington, A., Abrams, G. B., Barreira, P., & Kress, V. (2013). Nonsuicidal self-injury as a gateway to suicide in young adults. Journal of Adolescent Health, 52(4), 486-492.
Whitlock, J., & Rodham, K. (2013). Understanding nonsuicidal self-injury in youth. School Psychology Forum: Research in Practice, 7(4), 1-18.
World Health Organisation. (2014). Preventing suicide: A global imperative. Luxembourg: World Health Organisation.
You, J., Leung, F., Fu, K., & Lai, C. M. (2011). The prevalence of nonsuicidal self-injury and different subgroups of self-injurers in Chinese adolescents. Archives of Suicide Research, 15(1), 75-86.
Zubrick, S. R., Hafecost, J., Johnson, S., Lawrence, D., Saw, S., Sawyer, M. et al. (2016). Self-Harm: Prevalence estimates from Australia's Second Child and Adolescent Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry, 50(9), 911-921.
Zubrick, S. R., Hafecost, J., Johnson, S., Lawrence, D., Saw, S., Sawyer, M. et al. (2016). Suicidal behaviours: Prevalence estimates from Australia's Second Child and Adolescent Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry, 50(9), 899-910.
1 Using the LSAC data, Warren and Yu (2016) found that, particularly for girls, differences in pubertal status compared to peers, rather than the stage of pubertal development, are most problematic for emotional, social and school functioning; and these differences become less problematic as adolescents begin to reach a similar level of physical development.
2 Distal risk factors are background characteristics that may put someone at risk for an event or condition at some point in their lifetime (not immediately), while concurrent, or proximal, risk factors represent an immediate vulnerability.
3 A small proportion of adolescents did not answer questions related to self-harm and suicide-related behaviours either because parents or young people themselves did not give consent to be asked these questions (n = 56 and n = 4, respectively).
4 The original LSAC sample (Wave 1 sample) is not representative of very remote areas and immigrants.
5 Due to a small number of cases on key outcome variables, it was essential to binarise independent variables. Continuous variables were categorised into two groups using quartile scores (25% top/bottom vs the rest) with the top/bottom quartile classified as a higher/lower level of problems on a corresponding measure. Allocations to each subgroup were, therefore, relative to each other rather than being absolute measures.
6 Given that the outcome occurs in less than 10% of the unexposed population, the odds ratio provides a reasonable approximation of the relative risks ratios.
7 All risk factors included in Models 1 to 3 were tested in bivariate analysis and were significantly associated with an increased risk of self-harm and suicide attempts.