11. Eating problems in mid‑adolescence
11. Eating problems in mid‑adolescence

Overview
Being overweight and obese1 are risk factors for many serious and chronic health conditions and a major public health issue in Australia. Rates of being overweight and obese in Australia have risen over recent decades, with nearly two in three adults and one in four children considered to be overweight or obese in 2014-15 (Australian Bureau of Statistics [ABS], 2015). Estimates by the Australian Institute of Health and Welfare (AIHW; 2017) indicate that being overweight and obese were responsible for 7% of the total health burden in Australia in 2011, and in 2011-12, obesity was estimated to have cost the Australian economy $8.6 billion.
While rates of being overweight and obese are increasing, thin or even 'ultra-thin' bodies are often idealised in contemporary modern cultures, particularly for women. This ideal is unattainable for most and can generate body dissatisfaction and unhealthy eating behaviours (Thompson & Stice, 2001).
Eating problems cover a broad spectrum of issues ranging from anorexia nervosa and bulimia nervosa, which can be life threatening , to problematic eating behaviours such as restrictive dieting, which can represent a risk for the later development of eating disorders (Arcelus, Mitchell, Wales, & Nielsen, 2011; Stice, Shaw, & Marti, 2007). Once established, eating disorders are difficult to shift and can be a chronic problem affecting health and quality of life across the life span (Smink, van Hoeken, & Hoek, 2013).
Many eating problems develop in adolescence, with the peak incidence for anorexia nervosa and bulimia nervosa between the ages of 15 and 19 (Micali, Hagberg, Petersen, & Treasure, 2013). Therefore, intervening early, by promoting healthy eating and nutrition, when unhealthy eating behaviours start to arise is crucial for long-term health outcomes (Ciao, Loth, & Neumark-Sztainer, 2014).
The purpose of this chapter is to provide a 'snapshot' of how young people are faring in relation to eating problems at 14-15 years of age, the types of actions they take to control their weight and the association between those actions, particularly dieting, and physical and mental health outcomes.
11.1 Eating disorders
Eating disorders are characterised by abnormal eating behaviours and psychological disturbance related to food and weight. Abnormal eating behaviours include binge eating - consuming large amounts of food in a short period of time with a sense of loss of control - and other behaviours designed to rid oneself of food and/or control shape or weight. These other behaviours include self-induced vomiting, excessive exercise, laxative misuse, diet pills, diuretics and excessive dietary restriction (e.g. fasting, skipping meals and cutting out entire food groups) (The National Eating Disorders Collaboration [NEDC], 2010). Psychological disturbances related to food and weight may include an intense fear of becoming fat, disturbed body image, denial of the seriousness of low weight, and exaggerated emphasis on weight and shape in relation to one's self-worth (NEDC, 2010). The consequences of eating disorders can be severe, including poor quality of life (Jenkins, Hoste, Meyer, & Blissett, 2011), medical complications (Mitchell & Crow, 2006) and even death (Arcelus et al., 2011).
Estimates of the prevalence of eating disorders in Australia vary across studies, and Australian data are sparse. A South Australian population-based survey conducted in 2005 identified the lifetime prevalence of eating disorders as 0.3% for anorexia nervosa (80% female), 0.9% for bulimia nervosa (84% female) and 2.3% for binge eating disorder (67% female) (NEDC, 2010).
Box 11.1: Classification of eating disorders in the Branched Eating Disorders Test
In Wave 6 of LSAC, K cohort children completed a screening tool for eating disorders. The Branched Eating Disorders Test (BEDT) allows partial syndromal eating disorders to be identified. Partial syndromal eating disorders are identified where the young person has at least two of the three diagnostic criteria for anorexia nervosa or bulimia nervosa included in the Diagnostic and Statistical Manual - III R (Selzer, Hamill, Bowes, & Patton, 1996).
Respondents meeting two of the following three diagnostic criteria were classified as having partial syndromal bulimia nervosa:
- reporting their weight as being 'very important' to how they feel about themselves as a person
- reporting they have lost control of their eating or have eaten much too much at least weekly for at least three months
- reporting one of the following behaviours, lasting at least three months:
a.making themselves vomit as a means to control weight at least once per week
b.taking tablets, medicines or drugs to control their weight at least once per week
c.going all day without eating to control weight on four or more days per week
d.exercising in order to control weight six or seven days a week for two or more hours.
Respondents meeting two of the following diagnostic criteria were classified as having partial syndromal anorexia nervosa:
- being assessed as having a very low body weight, sourced from their Body Mass Index (BMI)
- reporting feeling afraid that they will gain weight on two to three days a week or more; reporting being 'very' or 'extremely' concerned about gaining weight; and being assessed as having a lower BMI than normal
- reporting their weight as being 'very important' to how they feel about themselves as a person; reporting themselves as being 'somewhat overweight' or 'very overweight'; and being assessed as having a lower BMI than normal
- reporting not having had their period in the last three months and not being pregnant at the time of interview (female respondents who have started menstruating only).
The LSAC data show that only a very small proportion of 14-15 year olds met the diagnostic criteria for partial syndromal anorexia nervosa or bulimia nervosa as measured by the BEDT ( Table 11.1 ).2 In particular, anorexia nervosa was extremely uncommon for both boys and girls, with less than half a percent meeting the diagnostic criteria. The proportion meeting the diagnostic criteria for bulimia nervosa was slightly higher, but still low, at 3% for girls and 1% for boys.
Notes: #Estimate not reliable (cell size < 20). n refers to complete case across variables.
Source: LSAC Wave 6, K cohort, weighted
Figure 11.1: Adolescents who met the diagnostic criteria for having anorexia nervosa or bulimia nervosa
11.2 Adolescents' feelings about their weight
While very few 14-15 year olds met the diagnostic criteria for an eating disorder, looking at responses to the individual components of the BEDT shows that many adolescents have negative feelings and beliefs about gaining weight. These feelings and actions can be problematic, even when the diagnostic criteria for an eating disorder are not met, and may reflect the early stages of an emerging disorder (Stice, Ng, & Shaw, 2010).
It was much more common for girls, than for boys, to say that they were afraid of gaining weight, or that they felt they had lost control of their eating. For example:
- Fifty-four per cent of girls and 19% of boys said that they had been afraid of gaining weight in the last four weeks.
- Forty-three per cent of girls and 20% of boys said that, in the last four weeks, they had felt that they had lost control of their eating or felt they had eaten too much.
Around 60% of 14-15 year olds (63% of boys and 56% of girls) said that, at the moment, they thought they were about the right weight (Figure 11.2). However, it was much more common for girls than boys to say that they felt somewhat overweight (33% compared to 19%), while boys more commonly said that they felt they were underweight.
When asked how they would feel if they gained one or two kilograms in weight, girls were much more concerned than boys (Figure 11.3). While around two thirds of girls said that they would be at least a little concerned and 15% said they would be really upset, more than 50% of boys said that gaining one or two kilograms would not bother them and 16% said that they would be pleased.
For a considerable proportion of girls, their weight was quite important to how they felt about themselves as a person. Just under 10% of girls said that it was not important, and one quarter said that it was very important (Figure 11.4). For boys, these figures were reversed, with only 11% saying their weight was very important for how they felt as a person, and 24% saying it was not important.
Figure 11.2: Feelings about their weight at age 14-15, by gender
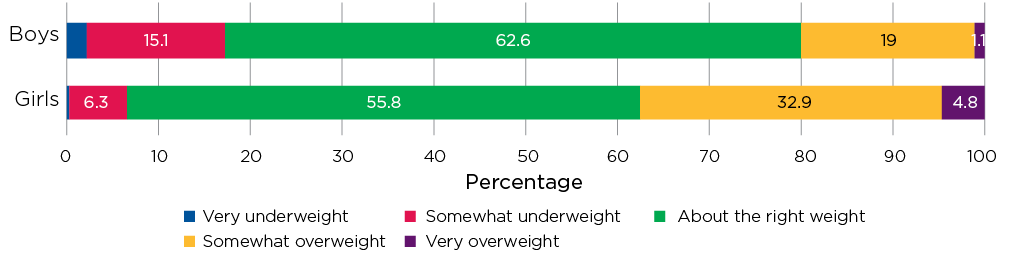
Note: n = 3,335.
Source: LSAC Wave 6, K cohort, weighted
Figure 11.3: Feelings about gaining one or two kilograms, age 14-15, by gender
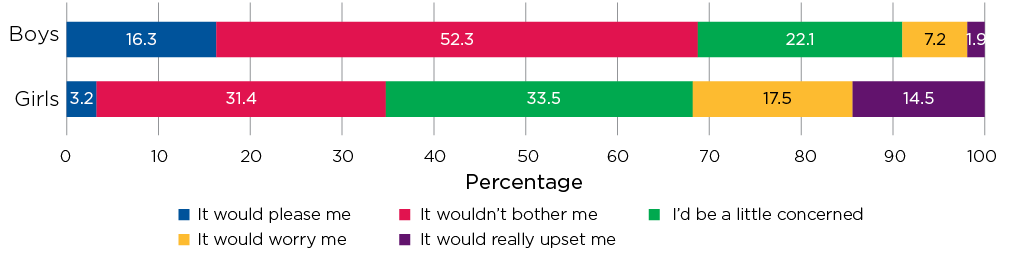
Note: n= 3,335.
Source: LSAC Wave 6, K cohort, weighted
Figure 11.4: Importance of weight in how you feel as a person, age 14-15, by gender
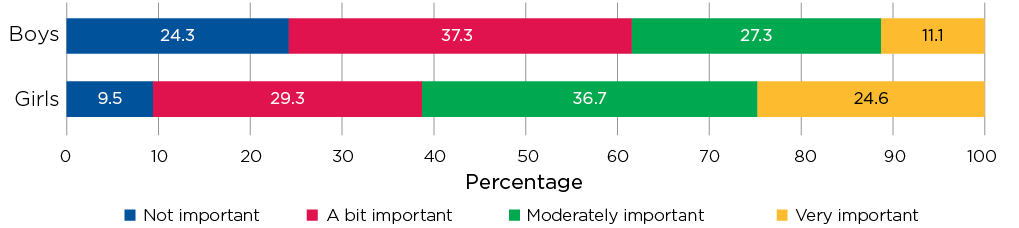
Note: n = 3,335.
Source: LSAC Wave 6, K cohort, weighted
These gender differences in their feelings and beliefs about gaining weight are likely to be at least partly due to societal expectations (Striegel-Moore & Bulik, 2007). The current beauty ideals in modern society promote a larger, more muscular build for men and, for women, a thin or even 'ultra-thin' ideal (Main, 2009). These standards are unachievable for most people, and the pressure to meet them can have many negative health effects (Paxton, 2000).
11.3 Actions taken to control weight
Given that many teens had expressed negative feelings about their weight, it is not surprising that some 14-15 year olds had reported taking some serious actions to control their weight, such as making themselves vomit or taking tablets, drugs or medicines. Among 14-15 year olds, 3% of girls, but less than 1% of boys, said that they had made themselves vomit at least once in the last four weeks in order to control their weight; and around 2% of boys and girls said they had taken some type of medicine.3
Exercise was a more common action taken to control weight; but most 14-15 year olds did not exercise at excessive levels. While 41% of girls and 58% of boys said that they had exercised at least once a week in the last four weeks to try to control their weight, only 3% of boys and 4% of girls were exercising for two or more hours per day, six or seven days per week (the diagnostic criteria for excessive exercise when assessing bulimia nervosa using the BEDT) (Figure 11.5). For most 14-15 year olds, exercising for the purposes of losing weight was not a regular habit, with only 17% of boys and 13% of girls reporting exercising at least four days per week for this purpose. Furthermore, most did not exercise for several hours at a time - around 16% of boys and girls said that, on days when they exercised to control their weight, they did so for two hours or more. It is important to keep in mind here that these figures include only exercise for the purposes of controlling weight - presumably some of those who reported not exercising to control their weight did exercise for other reasons, such as enjoyment and keeping fit, or as part of their school sport requirements.
Several large cross-sectional studies have investigated the frequency of specific weight control practices and found that fasting, skipping meals and using crash diets are quite common among teenagers (Canadian Pediatric Society, 2004). The LSAC data show that some 14-15 year olds (10% of girls and 6% of boys) reported having gone all day without eating at least once in the last four weeks. However, most teens did not do this frequently, with 32% of girls and 17% of boys who reported having gone all day without eating (less than 1% of all 14-15 year olds) doing so on two or more days per week.
Box 11.2: Adolescent dieting behaviours
In Wave 6 of LSAC, an adapted form of the Adolescent Dieting Scale4 (ADS) (Patton et al., 1997) was used for K cohort children (aged 14-15). Study children were asked how often they engaged in restrictive dieting by choosing 'Seldom/never', 'Sometimes', 'Often', or 'Almost always/always', in response to the following questions:
- Do you try to leave food at meal times in order to avoid putting on weight?
- When you have eaten too much, do you eat less than usual on the next day?
- Do you deliberately take small helpings at meals to keep your weight under control?
- Do you skip meals other than breakfast because you are watching your weight?
Figure 11.5: Exercise to control weight, at age 14-15, by gender
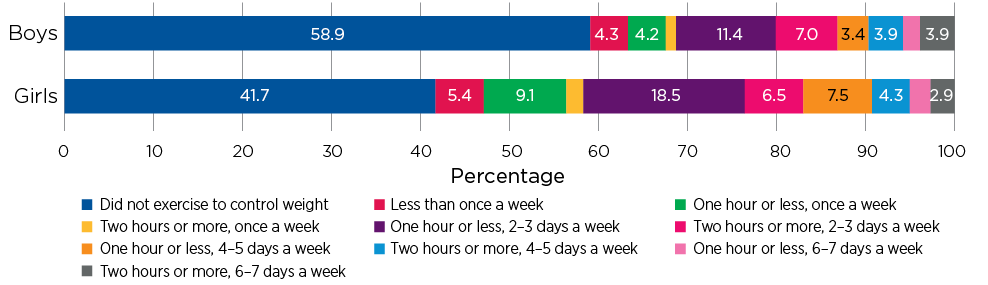
Note: n= 3,335.
Source: LSAC Wave 6, K cohort, weighted
While few teenagers reported taking extreme measures such as excessive exercise, making themselves vomit or taking tablets or other medicine to control their weight, dieting behaviours involving consciously restricting their food intake are relatively common in adolescence, particularly among girls.
For teenagers whose weight is within the healthy weight range, dieting may be used to maintain a healthy weight or to try to attain the thinner types of body shapes that are idealised in modern society (Patton et al., 1997). For young people who are overweight or obese, dieting might be considered a reasonable strategy to control or reduce their weight; however, focus on food quality, rather than food restriction, and a lifestyle approach to encourage enjoyable physical activity throughout the day is likely to be a better approach to maintaining a healthy weight (Ludwig, 2012).
Around a quarter of girls and 12% of boys reported engaging in some sort of dieting behaviour at age 14-15 (Table 11.2). These results were similar to the Healthy Neighbourhoods Study that, based on the published cut-offs for ADS, found 30% of adolescents aged 10-14 years were 'moderate/extreme dieters'. For girls and boys, the most common dieting behaviour was compensating for eating too much by eating less than usual the next day. This strategy was reported by 14% of girls and 7% of boys.
It was much more common for girls, than boys, to engage in dieting behaviour such as leaving food at meal times, deliberately taking small helpings, and skipping meals. Around 3% of boys reported doing each of these activities. The percentage of girls who engaged in these behaviours ranged from 9% for skipping meals to 12% deliberately taking small helpings at meal times.
Notes: Only percentages indicating the 'Often' or 'Almost always/Always' response options are shown. Other response options were 'Seldom/never' and 'Sometimes' and are not shown in the table.
Source: LSAC Wave 6, K cohort, weighted
11.4 Weight loss goals in early adolescence
For some adolescents, dieting at 14-15 years may be a continuation of behaviours that began much earlier. While there is no information about whether LSAC study children were engaging in dieting at age 10-11 or 12-13, previous research using LSAC has shown that even at age 10-11, almost 40% of boys and girls said that they were trying to lose weight (Daraganova, 2014).
Looking at the previous weight loss goals of adolescents who were dieting at age 14-15, it appears that for many teens, the desire to lose weight was an ongoing issue (Table 11.3). Over 40% of girls and boys who were dieting at age 14-15 had been consistently trying to lose weight since age 10-11; and a further 21% of girls and 16% of boys had been trying to lose weight since age 12-13 (Table 11.3).
Box 11.3: Weight change goals
At ages 10-11 and 12-13, LSAC study children were asked to 'pick the answer that shows what you are trying to do about your weight now' from the following options:
- lose weight
- gain weight
- stay the same weight
- I am not trying to do anything about my weight.
Note: Dieting behaviours include deliberately taking small helpings at meal times, skipping meals other than breakfast, leaving food at meal times in order to control weight, and eating less than usual in days when they feel they have eaten too much on the day before.
Source: LSAC Waves 4-6, K cohort, weighted
11.5 Dieting and wellbeing
Previous research has shown that most young people who diet are within a normal weight range (Patton et al., 1997). The LSAC data show that among 14-15 year olds who were dieting, around half of boys and 35% of girls were actually overweight, according to their Body Mass Index (Table 11.4). Over 60% of girls and 47% of boys were in the normal weight range; and a small proportion (less than 3%) were in fact underweight. This suggests that for many teens, and particularly for girls, the aim of their dieting is not to reduce their weight because they are overweight but to either maintain their weight within a healthy weight range or achieve a thinner body shape.
Notes: #Estimate not reliable, cell count < 20. Dieting behaviours include deliberately taking small helpings at meal times, skipping meals other than breakfast, leaving food at meal times in order to control weight, and eating less than usual in days when they feel they have eaten too much on the day before.
Source: LSAC Wave 6, K cohort, weighted
Box 11.4: Symptoms of anxiety
The Spence Children's Anxiety Scale (SCAS) is a self-report measure designed to assess the frequency with which children and adolescents experience anxiety symptoms (Spence, 1998; Spence, Barrett, & Turner, 2003). Study children were asked to rate on a four-point scale (with 0 meaning 'Never', 1 'Sometimes', 2 'Often' and 3 'Always') how often each of the following symptoms happen to them:
- I worry about things.
- I feel afraid.
- I feel afraid that I will make a fool of myself in front of people.
- I worry that something bad will happen to me.
- I feel nervous.
- I wake up feeling scared.
- I worry what other people think of me.
- All of a sudden, I feel really scared for no reason at all.
Responses were summed (ranging from 0 to 24), with scores of 11 or higher indicating elevated levels of anxiety.
Box 11.5: Symptoms of depression
The Short Mood and Feelings Questionnaire (SMFQ) is a brief self-report measure of symptoms of depression in children and adolescents (Sharp, Goodyer, & Croudace, 2006). The questionnaire consists of 13 items that require children to rate on a three-point scale ('True', 'Sometimes', and 'Not true') how much they consider a statement to be true of the way they have felt or acted in the past two weeks (e.g. 'I didn't enjoy anything at all.') Responses were summed, with a range from 0 to 26 and those with scores of 8 or higher were considered to have elevated depressive symptoms.
For some young people, eating behaviours and attitudes co-occur with mental health difficulties such as anxiety and depression (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011). Studies have shown that there is an overlap between the symptoms of eating problems and mental health difficulties; for example, a lack of appetite, lethargy and poor concentration are characteristics of both eating disorders and depression (Hughes et al., 2013). Eating problems can also lead to depression and anxiety through, for example, the effects of starvation and obsessive-compulsive behaviours related to food (Hughes et al., 2013).
The LSAC data show that, overall, girls who were dieting at age 14-15 had higher levels of emotional problems, compared to those who were not dieting (Table 11.5). Among girls who were dieting at age 14-15, 58% had elevated depressive symptoms and 47% had elevated symptoms of anxiety. For girls, symptoms of anxiety and depression were relatively common, even among those who were not engaging in any dieting behaviour, 27% had depressive symptoms and 19% had symptoms of anxiety.
Overall, symptoms of depression and anxiety were less common for boys than for girls. However, even for boys, there was a significant difference in the percentage with symptoms of anxiety or depression at age 14-15, depending on whether they were dieting. Among boys who were dieting, 32% had symptoms of depression and 16% had symptoms of anxiety. For boys who were not dieting, the corresponding percentages were lower: 17% with depression symptoms and 6% with symptoms of anxiety.
Eating problems can also have an impact on adolescents' functioning at school, their social lives, and physical health and development. There were relatively small but statistically significant differences in the average levels of emotional, school and social functioning; with lower levels among boys and girls who were dieting at age 14-15, compared to those who were not (Table 11.6).
In terms of physical health, there was not such a clear difference in functioning depending on whether children were dieting or not. For girls, average physical functioning scores were higher among those who were not dieting compared to those who were (75 compared to 69). However, this difference was not statistically significant. For boys, average physical functioning scores were quite similar (77 and 79 points), regardless of their dieting behaviour. This suggests that for most 14-15 year olds, their dieting habits are not related to their ability to participate in everyday activities.
Notes: Dieting behaviours include deliberately taking small helpings at meal times, skipping meals other than breakfast, leaving food at meal times in order to control weight, and eating less than usual in days when they feel they have eaten too much on the day before.
Source: LSAC Wave 6, K cohort, weighted
Notes: Higher scores indicate better functioning in that domain. Emotional, social and school functioning measures were based on the PedsQL Pediatric Quality of Life Scale; and physical health was based on the PedsQL Teen Physical Health Scale. Dieting behaviours include deliberately taking small helpings at meal times, skipping meals other than breakfast, leaving food at meal times in order to control weight, and eating less than usual in days when they feel they have eaten too much on the day before.
Source: LSAC Wave 6, K cohort, weighted
Box 11.6: The Pediatric Quality of Life Inventory (PedsQL)
Adolescents' emotional, school and social functioning and peer relationships were measured using the Pediatric Quality of Life (PedsQL) inventory (Varni, Burwinkle, & Seid, 2006).
Emotional functioning assesses the frequency that the child displays negative emotional states such as sadness and anxiety. Parents were asked how often the study child had the following problems in the past month:
- feeling afraid or scared
- feeling sad or blue
- feeling angry
- trouble sleeping
- worry about what will happen to him/her.
School functioning measures children's school adjustment and performance. Parents were asked how often the study child had the following problems in the past month:
- paying attention in class
- forgetting things
- keeping up with school activities
- missing school because of not feeling well
- missing school to go to doctor or hospital.
Social functioning assesses children's relationship with their peers. Parents were asked to rate how frequently the study child had the following problems in the past month:
- getting along with other children
- other kids not wanting to be his/her friend
- getting teased by other children
- not being able to do things that other children his/her age can do
- keeping up when playing with other children.
The study child's primary caregiver (in most cases their mother) was asked to rate each item on a five-point scale, ranging from 1 (Never) to 5 (Almost always). Items were reverse-scored and transformed to a 0-100 scale (1 = 100, 2 = 75, 3 = 50, 4 = 25, 5 = 0), so that higher scores indicated a higher level of functioning. Average scores were then calculated to create the emotional, school and social functioning subscales.
Box 11.7: The PedsQL Teen Physical Health Scale
Adolescents' levels of physical functioning were measured using the teen physical health scale. Study children were asked how often the following activities have been difficult for them in the last month:
- walk more than 100 metres
- run
- play sport or do exercise
- lift something heavy
- have a bath or shower by myself
- help around the house.
As well as how often they:
- get aches and pains
- have low energy.
LSAC study children were asked to rate each item on a five-point scale, ranging from 0 (Never) to 4 (Almost always). Items were reverse-scored and transformed to a 0-100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0), so that higher scores indicated a higher level of functioning. Average scores were then calculated to create the teen physical health scale.
Summary
This chapter provides a description of how young people are faring in relation to eating problems at 14-15 years of age. The LSAC data show that few 14-15 year olds partially fulfil the diagnostic criteria for an eating disorder. However, the prevalence of eating disorders among LSAC study children is likely to increase when they are in their late teens, as peak incidence for anorexia nervosa and bulimia nervosa occurs between the ages of 15 and 19 (Micali et al., 2013).
Eating disorders such as bulimia nervosa and anorexia nervosa can be understood as reflecting the extreme end of a continuum, and many young people experience milder eating problems that do not meet diagnostic criteria (Xiaochen, 2016). Even if these milder eating problems do not progress to an eating disorder, they are still problematic because they can be distressing to the individual and affect their daily lives (Stice, Marti, Shaw, & Jaconis, 2009).
The LSAC data show that, among 14-15 year olds, negative feelings about weight, and taking actions to try to control weight, are much more common than eating disorders; and more common for girls than for boys. For example, 54% of girls and 19% of boys said that they had been afraid of gaining weight in the last four weeks. In terms of actions taken to control weight, diet and exercise were much more common than drastic actions such as taking diet pills or vomiting after meals.
Almost a quarter of girls and 12% of boys reported consciously restricting their food intake at age 14-15. Among those who did engage in some type of dieting, a high proportion (63% of girls and 47% of boys) were in the average weight range according to their BMI. This suggests that for most teens, the reason for dieting is not to reduce weight because they are overweight, but to either maintain their weight within the healthy weight range or achieve the thinner types of body shapes that are typically idealised in our society.
Overall, girls seemed to be faring worse in relation to eating problems than boys. They had a higher prevalence of both eating disorders and dieting behaviours. The number of boys with eating problems was not negligible, however, so their eating problems should not be ignored (Calzo et al., 2016).
For some adolescents who were dieting at age 14-15, their desire to lose weight traces back to early adolescence. The proportion of those who were dieting at 14-15 years was higher among those who had also been trying to lose weight at 10-11 and 12-13 years than those who had not. This type of information can help us to understand more about who to target for early prevention efforts and what factors to target (Le Grange et al., 2014; Stice et al., 2010). It reinforces that we can begin prevention efforts early on, including in late childhood and early adolescence.
The analysis in this chapter also supports the findings of other studies showing that anxiety and depression often occur in combination with eating problems. Therefore, it is important to address both together (Hughes et al., 2013). Levels of emotional, school and social functioning are also lower among boys and girls who were engaging in dieting at age 14-15, compared to those who were not. However, for 14-15 year olds, it appears that restrictive dieting is related to poorer functioning in some aspects of their lives more so than others. In terms of physical functioning, those who were engaging in restrictive dieting were not faring any worse, on average, than those who were not.
Further research using the LSAC data to identify the characteristics or circumstances of individuals who are most at risk of eating problems, and the factors that are likely to shift outcomes for this high risk group, would be very useful for health practitioners, particularly for informing the development of prevention and intervention approaches.
References
Arcelus, J., Mitchell, A. J., Wales, J., & Nielsen, S. (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry, 68(7), 724-731. doi: 10.1001/archgenpsychiatry.2011.74
Australian Bureau of Statistics (ABS). (2015). National Health Survey: First results, 2014-15. Canberra: ABS.
Australian Institute of Health and Welfare (AIHW). (2017). A picture of overweight and obesity in Australia 2017. Cat. no. PHE 216. Canberra: AIHW.
Calzo, J. P., Horton, N. J., Sonneville, K. R., Swanson, S. A., Crosby, R. D., Micali, N. et al. (2016). Male eating disorder symptom patterns and health correlates from 13 to 26 years of age. Journal of the American Academy of Child & Adolescent Psychiatry, 55(8), 693-700. e692.
Ciao, A. C., Loth, K., & Neumark-Sztainer, D. (2014). Preventing eating disorder pathology: Common and unique features of successful eating disorders prevention programs. New York: Springer.
Daraganova, G. (2014). Body image of primary school children. In Australian Institute of Family Studies (Ed.). The Longitudinal Study of Australian Children annual statistical report 2013 (pp. 111-134). Melbourne: AIFS.
Hughes, E. K., Goldschmidt, A. B., Labuschagne, Z., Loeb, K. L., Sawyer, S. M., & Grange, D. L. (2013). Eating disorders with and without comorbid depression and anxiety: Similarities and differences in a clinical sample of children and adolescents. European Eating Disorders Review, 21(5), 386-394.
Jenkins, P. E., Hoste, R. R., Meyer, C., & Blissett, J. M. (2011). Eating disorders and quality of life: A review of the literature. Clinical Psychology Review, 31(1), 113-121.
Le Grange, D., O'Connor, M., Hughes, E. K., Macdonald, J., Little, K., & Olsson, C. A. (2014). Developmental antecedents of abnormal eating attitudes and behaviors in adolescence. The International Journal Of Eating Disorders, 47(7), 813-824. doi: 10.1002/eat.22331
Ludwig, D. S. (2012). Weight loss strategies for adolescents: A 14 year old struggling to lose weight. JAMA, 307(5), 498-508.
Main, A. (2009). Gender impact assessment: Body image. Melbourne: Womens Health Victoria. Retrieved from whv.org.au/static/files/assets/3aabe075/bodyimage-gia.pdf
Micali, N., Hagberg, K. W., Petersen, I., & Treasure, J. L. (2013). The incidence of eating disorders in the UK in 2000-2009: Findings from the General Practice Research Database. BMJ Open, 3(5), e002646.
Mitchell, J. E., & Crow, S. (2006). Medical complications of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry, 19(4), 438-443. doi: 10.1097/01.yco.0000228768.79097.3e
The National Eating Disorders Collaboration (NEDC). (2010). Eating disorders: The way forward. An Australian national framework. Sydney: NEDC.
Patton, G. C., Carlin, J., Shao, Q., Hibbert, M., Rosier, M., Selzer, R., & Bowes, G. (1997). Adolescent dieting: healthy weight control or borderline eating disorder? Journal of Child Psychology and Psychiatry, 38(3), 299-306.
Paxton, S. J. (2000). Body image dissatisfaction, extreme weight loss behaviours: Suitable targets for public health concern? Health Promotion Journal of Australia, 10(1), 15-19.
Selzer, R., Hamill, C., Bowes, G., & Patton, G. (1996). The Branched Eating Disorders Test: Validity in a nonclinical population. International Journal of Eating Disorders, 20(1), 57-62.
Sharp, C., Goodyer, I. M., & Croudace, T. J. (2006). The Short Mood and Feelings Questionnaire (SMFQ): A unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7- through 11-year-old children. Journal of Abnormal Child Psychology, 34(3), 365-377. doi: 10.1007/s10802-006-9027-x
Smink, F. R., van Hoeken, D., & Hoek, H. W. (2013). Epidemiology, course, and outcome of eating disorders. Current Opinion in Psychiatry, 26(6), 543-548.
Spence, S. H. (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36(5), 545-566.
Spence, S. H., Barrett, P. M., & Turner, C. M. (2003). Psychometric properties of the Spence Children's Anxiety Scale with young adolescents. Journal of Anxiety Disorders, 17(6), 605-625.
Stice, E., Marti, C. N., Shaw, H., & Jaconis, M. (2009). An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology, 118(3), 587-597. doi: 10.1037/a0016481
Stice, E., Ng, J., & Shaw, H. (2010). Risk factors and prodromal eating pathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 51(4), 518-525. doi: 10.1111/j.1469-7610.2010.02212.x
Stice, E., Shaw, H., & Marti, C. N. (2007). A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annual Review of Clinical Psychology, 3, 207-231.
Striegel-Moore, R. H., & Bulik, C. M. (2007). Risk factors for eating disorders. American Psychologist, 62(3), 181.
Swanson, S. A., Crow, S. J., Le Grange, D., Swendsen, J., & Merikangas, K. R. (2011). Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68(7), 714-723. doi: 10.1001/archgenpsychiatry.2011.22
Thompson, J. K., & Stice, E. (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10(5), 181-183.
Varni, J. W., Burwinkle, T. M., & Seid, M. (2016). The PedsQLTM 4.0 as a school population health measure: Feasibility, reliability, and validity. Quality of Life Research, 15, 203-215.
Xiaochen, L. (2016). The dimensional nature of eating pathology: Evidence from a direct comparison of categorical, dimensional, and hybrid models. Journal of Abnormal Psychology, 125(5), 715.
1 Addressing overweight and obesity is a national health priority. Obesity campaigns and publications often focus on changing thoughts and behaviours related to eating and weight. In addressing these issues, care must be taken not to cause unintended harm. Young people in larger bodies are at higher risk of disordered eating and eating disorders than the general population. Awareness-raising initiatives focusing on obesity in children and young people, without appropriate information and support for effective lifestyle changes, may be misinterpreted by children, young people and their parents as cues to engage in dieting, such as fad or restrictive dieting. This is unsuitable for growing children and may have detrimental consequences for health and physical growth. For more information about the Key Principles and Assumptions for Weight‑Related Public Health Messages on the National Eating Disorders Collaboration website.
2 Note that not all the eating disorders described in the Diagnostic and Statistical Manual of Mental Disorders (DSM) (2013) (e.g. binge eating disorder (BED), other specified feeding and eating disorders (OSFED) and unspecified feeding and eating disorders (UFED)) can be identified using the BEDT.
3 Study children were asked the types of medicines that they had taken to control their weight (e.g. laxatives, diuretics, appetite suppressants or other drugs) and how often they took these medications. However, the number of observations for those who reported taking medicines to control their weight was too small for reliable estimates of the specific types of medicines used.
4 Only four of eight original items were asked in LSAC with the wording of the original items being slightly modified.
Acknowledgements
Featured image: © GettyImages/Steve Debenport